Enhancing Public Health Preparedness for Climate Change-Related Health Impacts
The escalating frequency and intensity of extreme heat events, exacerbated by climate change, pose a significant and growing threat to public health. This problem is further compounded by the lack of standardized education and preparedness measures within the healthcare system, creating a critical gap in addressing the health impacts of extreme heat. The Department of Health and Human Services (HHS), especially the Centers for Medicare & Medicaid Services (CMS), the Health Resources and Services Administration (HRSA), and the Office of Climate Change and Health Equity (OCCHE) can enhance public health preparedness for the health impacts of climate change. By leveraging funding mechanisms, incentives, and requirements, HHS can strengthen health system preparedness, improve health provider knowledge, and optimize emergency response capabilities.
By focusing on interagency collaboration and medical education enhancement, strategic measures within HHS, the healthcare system can strengthen its resilience against the health impacts of extreme heat events. This will not only improve coding accuracy, but also enhance healthcare provider knowledge, streamline emergency response efforts, and ultimately mitigate the health disparities arising from climate change-induced extreme heat events. Key recommendations include: establishing dedicated grant programs and incentivizing climate-competent healthcare providers; integrating climate-resilience metrics into quality measurement programs; leveraging the Health Information Technology for Economic and Clinical Health (HITECH) Act to enhance ICD-10 coding education; and collaborating with other federal agencies such as the Department of Veterans Affairs (VA), the Federal Emergency Management Agency (FEMA), and the Department of Defense (DoD) to ensure a coordinated response. The implementation of these recommendations will not only address the evolving health impacts of climate change but also promote a more resilient and prepared healthcare system for the future.
Challenge
The escalating frequency and intensity of extreme heat events, exacerbated by climate change, pose a significant and growing threat to public health. The scientific consensus, as documented by reports from the Intergovernmental Panel on Climate Change (IPCC) and the National Climate Assessment, reveals that vulnerable populations, such as children, pregnant people, the elderly, and marginalized communities including people of color and Indigenous populations, experience disproportionately higher rates of heat-related illnesses and mortality. The Lancet Countdown’s 2023 U.S. Brief underscores the escalating threat of fossil fuel pollution and climate change to health, highlighting an 88% increase in heat-related mortality among older adults and calling for urgent, equitable climate action to mitigate this public health crisis.
Inadequacies in Current Healthcare System Response
Reports from healthcare institutions and public health agencies highlight how current coding practices contribute to the under-recognition of heat-related health impacts in vulnerable populations, exacerbating existing health disparities. The current inadequacies in ICD-10 coding for extreme heat-related health cases hinder effective healthcare delivery, compromise data accuracy, and impede the development of targeted response strategies. Challenges in coding accuracy are evident in existing studies and reports, emphasizing the difficulties healthcare providers face in accurately documenting extreme heat-related health cases. An analysis of emergency room visits during heat waves further indicates a gap in recognition and coding, pointing to the need for improved medical education and coding practices. Audits of healthcare coding practices reveal inconsistencies and inaccuracies that stem from a lack of standardized medical education and preparedness measures, ultimately leading to underreporting and misclassification of extreme heat cases. Comparative analyses of health data from regions with robust coding practices and those without highlight the disparities in data accuracy, emphasizing the urgent need for standardized coding protocols.
There is a crucial opportunity to enhance public health preparedness by addressing the challenges associated with accurate ICD-10 coding in extreme heat-related health cases. Reports from government agencies and economic research institutions underscore the economic toll of extreme heat events on healthcare systems, including increased healthcare costs, emergency room visits, and lost productivity due to heat-related illnesses. Data from social vulnerability indices and community-level assessments emphasize the disproportionate impact of extreme heat on socially vulnerable populations, highlighting the urgent need for targeted policies to address health disparities.
Opportunity
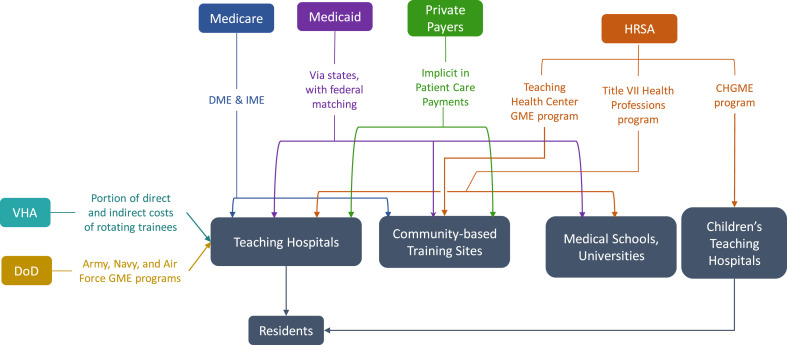
As Medicare is the largest federal source of Graduate Medical Education (GME) funding (Figure 1), the Department of Health and Human Services’ (HHS) Centers for Medicare & Medicaid Services (CMS) and the National Center for Health Statistics (NCHS) play a critical role in developing coding guidelines. Thus, it is essential for HHS, CMS, and other pertinent coordinating agencies to be involved in the process for developing climate change-informed graduate medical curricula.
By focusing on medical education enhancement, strategic measures within HHS, and fostering interagency collaboration, the healthcare system can strengthen its resilience against the health impacts of extreme heat events. Improving coding accuracy, enhancing healthcare provider knowledge, streamlining emergency response efforts, and mitigating health disparities related to extreme heat events will ultimately strengthen the healthcare system and foster more effective, inclusive, and equitable climate and health policies. Improving the knowledge and training of healthcare providers empowers them to respond more effectively to extreme heat-related health cases. This immediate response capability contributes to the overarching goal of reducing morbidity and mortality rates associated with extreme heat events and creates a public health system that is more resilient and prepared for emerging challenges.
The inclusion of ICD-10 coding education into graduate medical education funded by CMS aligns with the precedent set by the Pandemic and All Hazards Preparedness Act (PAHPA), emphasizing the importance of preparedness and response to public health emergencies. Similarly, drawing inspiration from the Health Information Technology for Economic and Clinical Health Act (HITECH Act), which promotes the adoption of electronic health records (EHR) systems, presents an opportunity to modernize medical education and ensure the seamless integration of climate-related health considerations. This collaborative and forward-thinking approach recognizes the interconnectedness of health and climate, offering a model that can be applied to various health challenges. Integrating mandates from PAHPA and the HITECH Act serves as a policy precedent, guiding the healthcare system toward a more adaptive and proactive stance in addressing climate change impacts on health.
Conversely, the consequences of inaction on the health impacts of extreme heat extend beyond immediate health concerns. They permeate through the fabric of society, widening health disparities, compromising the accuracy of health data, and undermining emergency response preparedness. Addressing these challenges requires a proactive and comprehensive approach to ensure the well-being of communities, especially those most vulnerable to the effects of extreme heat.
Plan of Action
The following recommendations aim to facilitate public health preparedness for extreme heat events through enhancements in medical education, strategic measures within the Department of Health and Human Services (HHS), and fostering interagency collaboration.
Recommendation 1a. Integrate extreme heat training into the GME curriculum.
Integrating modules on extreme heat-related health impacts and accurate ICD-10 coding into medical education curricula is essential for preparing future healthcare professionals to address the challenges posed by climate change. This initiative will ensure that medical students receive comprehensive training on identifying, treating, and documenting extreme heat-related health cases. Sec. 304. Core Education and Training of the PAHPA provides policy precedent to develop foundational health and medical response curricula and training materials by modifying relevant existing programs to enhance responses to public health emergencies. Given the prominence of Medicare in funding medical residency training, policies that alter Medicare GME can affect the future physician supply and can be used to address identified healthcare workforce priorities related to extreme heat (Figure 2).
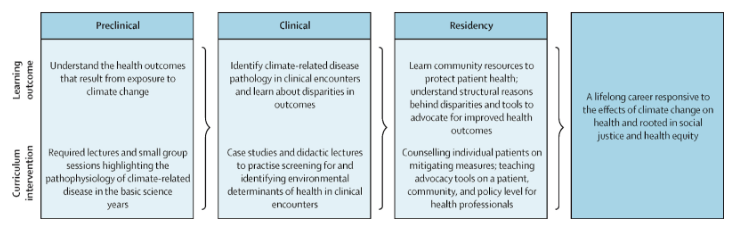
Figure 2: A model for comprehensive climate and medical education (adapted from Jowell et al. 2023)
Recommendation 1b. Collaborate with Veterans Health Administration Training Programs.
Partnering with the Department of Veterans Affairs (VA) to extend climate-related health coding education to Veterans Health Administration (VHA) training programs will enhance the preparedness of healthcare professionals within the VHA system to manage and document extreme heat-related health cases among veteran populations.
Recommendation 2. Collaborate with the Agency for Healthcare Research and Quality (AHRQ)
Establishing a collaborative research initiative with the Agency for Healthcare Research and Quality (AHRQ) will facilitate the in-depth exploration of accurate ICD-10 coding for extreme heat-related health cases. This should be accomplished through the following measures:
Establish joint task forces. CMS, NCHS, and AHRQ should establish joint research initiatives focused on improving ICD-10 coding accuracy for extreme heat-related health cases. This collaboration will involve identifying key research areas, allocating resources, and coordinating research activities. Personnel from each agency, including subject matter experts and researchers from the EPA, NOAA, and FEMA, will work together to conduct studies, analyze data, and publish findings. By conducting systematic reviews, developing standardized coding algorithms, and disseminating findings through AHRQ’s established communication channels, this initiative will improve coding practices and enhance healthcare system preparedness for extreme heat events.
Develop standardized coding algorithms. AHRQ, in collaboration with CMS and NCHS, will lead efforts to develop standardized coding algorithms for extreme heat-related health outcomes. This involves reviewing existing coding practices, identifying gaps and inconsistencies, and developing standardized algorithms to ensure consistent and accurate coding across healthcare settings. AHRQ researchers and coding experts will work closely with personnel from CMS and NCHS to draft, validate, and disseminate these algorithms.
Integrate into Continuous Quality Improvement (CQI) programs. Establish collaborative partnerships between the VA and other federal healthcare agencies, including CMS, HRSA, and DoD, to integrate education on ICD-10 coding for extreme heat-related health outcomes into CQI programs. Regularly assess the effectiveness of training initiatives and adjust based on feedback from healthcare providers. For example, CMS currently requires physicians to screen for the social determinants of health and could include level of climate and/or heat risk within that screening assessment.
Allocate resources. Each agency will allocate financial resources, staff time, and technical expertise to support collaborative activities. Budget allocations will be based on the scope and scale of specific initiatives, with funds earmarked for research, training, data sharing, and evaluation efforts. Additionally, research funding provided through PHSA Titles VII and VIII can support studies evaluating the effectiveness of educational interventions on climate-related health knowledge and practice behaviors among healthcare providers.
Recommendation 3. Leverage the HITECH Act and EHR.
Recommendation 4. Establish climate-resilient health system grants to incentivize state-level climate preparedness initiatives
HHS and OCCHE should create competitive grants for states that demonstrate proactive climate change adaptation efforts in healthcare. These agencies can encourage states to integrate climate considerations into their health plans by providing additional funding to states that prioritize climate resilience.
Within CMS, the Center for Medicare and Medicaid Innovation (CMMI) could help create and administer these grants related to climate preparedness initiatives. Given its focus on innovation and testing new approaches, CMMI could design grant programs aimed at incentivizing state-level climate resilience efforts in healthcare. Given its focus on addressing health disparities and promoting preventive care, the Bureau of Primary Health Care (BPHC) within HRSA could oversee grants aimed at integrating climate considerations into primary care settings and enhancing resilience among vulnerable populations.
Conclusion
These recommendations provide a comprehensive framework for HHS — particularly CMS, HRSA, and OCCHE— to bolster public health preparedness for the health impacts of extreme heat events. By leveraging funding mechanisms, incentives, and requirements, HHS can enhance health system preparedness, improve health provider knowledge, and optimize emergency response capabilities. These strategic measures encompass a range of actions, including establishing dedicated grant programs, incentivizing climate-competent healthcare providers, integrating climate-resilience metrics into quality measurement programs, and leveraging the HITECH Act to enhance ICD-10 coding education. Collaboration with other federal agencies further strengthens the coordinated response to the growing challenges posed by climate change-induced extreme heat events. By implementing these policy recommendations, HHS can effectively address the evolving landscape of climate change impacts on health and promote a more resilient and prepared healthcare system for the future.
This idea of merit originated from our Extreme Heat Ideas Challenge. Scientific and technical experts across disciplines worked with FAS to develop potential solutions in various realms: infrastructure and the built environment, workforce safety and development, public health, food security and resilience, emergency planning and response, and data indices. Review ideas to combat extreme heat here.
- Improved Accuracy in ICD-10 Coding: Healthcare providers consistently apply accurate ICD-10 coding for extreme heat-related health cases.
- Enhanced Healthcare Provider Knowledge: Healthcare professionals possess comprehensive knowledge on extreme heat-related health impacts, improving patient care and response strategies.
- Strengthened Public Health Response: A coordinated effort results in a more effective and equitable public health response to extreme heat events, reducing health disparities.
- Improved Public Health Resilience:
- Short-Term Outcome: Healthcare providers, armed with enhanced knowledge and training, respond more effectively to extreme heat-related health cases.
- Long-Term Outcome: Reduced morbidity and mortality rates associated with extreme heat events lead to a more resilient and prepared public health system.
- Enhanced Data Accuracy and Surveillance:
- Short-Term Outcome: Improved accuracy in ICD-10 coding facilitates more precise tracking and surveillance of extreme heat-related health outcomes.
- Long-Term Outcome: Comprehensive and accurate data contribute to better-informed public health policies, targeted interventions, and long-term trend analysis.
- Reduced Health Disparities:
- Short-Term Outcome: Incentives and education programs ensure that healthcare providers prioritize accurate coding, reducing disparities in the diagnosis and treatment of extreme heat-related illnesses.
- Long-Term Outcome: Health outcomes become more equitable across diverse populations, mitigating the disproportionate impact of extreme heat on vulnerable communities.
- Increased Public Awareness and Education:
- Short-Term Outcome: Public health campaigns and educational initiatives raise awareness about the health risks associated with extreme heat events.
- Long-Term Outcome: Informed communities adopt preventive measures, reducing the overall burden on healthcare systems and fostering a culture of proactive health management.
- Streamlined Emergency Response and Preparedness:
- Short-Term Outcome: Integrating extreme heat preparedness into emergency response plans results in more efficient and coordinated efforts during heatwaves.
- Long-Term Outcome: Improved community resilience, reduced strain on emergency services, and better protection for vulnerable populations during extreme heat events.
- Increased Collaboration Across Agencies:
- Short-Term Outcome: Collaborative efforts between OCCHE, CMS, HRSA, AHRQ, FEMA, DoD, and the Department of the Interior result in streamlined information sharing and joint initiatives.
- Long-Term Outcome: Enhanced cross-agency collaboration establishes a model for addressing complex public health challenges, fostering a more integrated and responsive government approach.
- Empowered Healthcare Workforce:
- Short-Term Outcome: Incentives for accurate coding and targeted education empower healthcare professionals to address the unique challenges posed by extreme heat.
- Long-Term Outcome: A more resilient and adaptive healthcare workforce is equipped to handle emerging health threats, contributing to overall workforce well-being and satisfaction.
- Informed Policy Decision-Making:
- Short-Term Outcome: Policymakers utilize accurate data and insights to make informed decisions related to extreme heat adaptation and mitigation strategies.
- Long-Term Outcome: The integration of health data into broader climate and policy discussions leads to more effective, evidence-based policies at local, regional, and national levels.
A deeper understanding of methane could help scientists better address these impacts – including potentially through methane removal.
We are encouraged that the Administration and Congress are recognizing the severity of the wildfire crisis and elevating it as a national priority. Yet the devil is in the details when it comes to making real-world progress.
The good news is that even when the mercury climbs, heat illness, injury, and death are preventable. The bad news is that over the past five months, the Trump administration has dismantled essential preventative capabilities.
The Federation of American Scientists supports H.Res. 446, which would recognize July 3rd through July 10th as “National Extreme Heat Awareness Week”.