Supporting Federal Decision Making through Participatory Technology Assessment
The incoming administration needs a robust, adaptable and scalable participatory assessment capacity to address complex issues at the intersections of science, technology, and society. As such, the next administration should establish a special unit within the Science and Technology Policy Institute (STPI)—an existing federally funded research and development center (FFRDC)—to provide evidence-based, just-in-time, and fit-for-purpose capacity for Participatory Technology Assessment (pTA) to the White House Office of Science and Technology Policy and across executive branch agencies.
Robust participatory and multi-stakeholder engagement supports responsible decision making where neither science nor existing policy provide clear guidance. pTA is an established and evidence-based process to assess public values, manage sociotechnical uncertainties, integrate living and lived knowledge, and bridge democratic gaps on contested and complex science and society issues. By tapping into broader community expertise and experiences, pTA identifies plausible alternatives and solutions that may be overlooked by experts and advocates.
pTA provides critical and informed public input that is currently missing in technocratic policy- and decision-making processes. Policies and decisions will have greater legitimacy, transparency, and accountability as a result of enhanced use of pTA. When systematically integrated into research and development (R&D) processes, pTA can be used for anticipatory governance—that is, assessing socio-technical futures, engaging communities, stakeholders and publics, and directing decisions, policies, and investments toward desirable outcomes.
A pTA unit within STPI will help build and maintain a shared repository of knowledge and experience of the state of the art and innovative applications across government, and provide pTA as a design, development, implementation, integration and training service for the executive branch regarding emerging scientific and technological issues and questions. By integrating public and expert value assessments, the next administration can ensure that federal science and technology decisions provide the greatest benefit to society.
Challenge and Opportunity
Science and technology (S&T) policy problems always involve issues of public values—such as concerns for safety, prosperity, and justice—alongside issues of fact. However, few systematic and institutional processes meaningfully integrate values from informed public engagement alongside expert consultation. Existing public-engagement mechanisms such as public- comment periods, opinion surveys, and town halls have devolved into little more than “checkbox” exercises. In recent years, transition to online commenting, intended to improve access and participation, have also amplified the negatives. They have “also inadvertently opened the floodgates to mass comment campaigns, misattributed comments, and computer-generated comments, potentially making it harder for agencies to extract the information needed to inform decision making and undermining the legitimacy of the rulemaking process. Many researchers have found that a large percentage of the comments received in mass comment responses are not highly substantive, but rather contain general statements of support or opposition. Commenters are an entirely self selected group, and there is no reason to believe that they are in any way representative of the larger public. … Relatedly, the group of commenters may represent a relatively privileged group, with less advantaged members of the public less likely to engage in this form of political participation.”
Moreover, existing engagement mechanisms tend to be dominated by a small number of experts and organized interest groups: people and institutions who generally have established pathways to influence policy anyway.
Existing engagement mechanisms leave out the voices of people who may lack the time, awareness, and/or resources to voice their opinions in response to the Federal Register, such as the roofer, the hair stylist, or the bus driver. This means that important public values—widely held ideas about the rights and benefits that ought to guide policy making in a democratic system—go overlooked. For S&T policy, a failure to assess and integrate public values may result in lack of R&D and complementary investments that produce market successes with limited public value, such as treatments for cancer that most patients cannot afford or public failure when there is no immediately available technical or market response, such as early stages of a global pandemic. Failure to integrate public values may also mean that little to no attention gets paid to key areas of societal need, such as developing low-cost tools and approaches for mitigating lead and other contaminants in water supplies or designing effective policy response, such as behavioral and logistical actions to contain viral infections and delivering vaccination to resistant populations.
In its 2023 Letter to the President, the President’s Council of Advisors on Science and Technology (PCAST), observed that, “As a nation, we must strive to develop public policies that are informed by scientific understandings and community values. Achieving this goal will require both access to accurate and trusted scientific information and the ability to create dialogue and participatory engagement with the American people.” The PCAST letter recommends issuing “a clarion call to Federal agencies to make science and technology communication and public engagement a core component of their mission and strategy.” It also recommended the establishment of “a new office to support Federal agencies in their continuing efforts to develop and build participatory public engagement and effective science and technology communications.”
Institutionalizing pTA within the Federal Government would provide federal agencies access to the tools and resources they need to apply pTA to existing and emerging complex S&T challenges, enabling experts, publics, and decision makers to tackle pressing issues together.pTA can be applied toward resolving long-standing issues, as well as to anticipate and address questions around emerging or novel S&T issues.
pTA for Long-Standing S&T Issues
Storage and siting of disposal sites for nuclear waste is an example of the type of ongoing, intractable problems for which pTA is ideally suited. Billions of dollars have been invested to develop a government-managed site for storing nuclear waste in the United States, yet essentially no progress has been made. Entangled political and environmental concerns, such as the risks of leaving nuclear waste in a potentially unsafe state for the long term, have stalled progress. There is also genuine uncertainty and expert disagreement surrounding safety and efficacy of various storage alternatives. Our nation’s inability to address the issue of nuclear waste has long impacted development of new and alternative nuclear power plants and thus has contributed to the slowing the adoption of nuclear energy.
There are rarely unencumbered or obvious optimal solutions to long-standing S&T issues like nuclear-waste disposal. But a nuanced and informed dialogue among a diverse public, experts, and decision makers—precisely the type of dialogue enabled through pTA—can help break chronic stalemates and address misaligned or nonexistent incentives. By bringing people together to discuss options and to learn about the benefits and risks of different possible solutions, pTA enables stakeholders to better understand each other’s perspectives. Deliberative engagements like pTA often generate empathy, encouraging participants to collaborate and develop recommendations based on shared exploration of values. pTA is designed to facilitate timely, adequate, and pragmatic choices in the context of uncertainty, conflicting goals, and various real-world constraints. This builds transparency and trust across diverse stakeholders while helping move past gridlock.
pTA for Emerging and Novel Issues
pTA is also useful for anticipating controversies and governing emerging S&T challenges, such as the ethical dimensions of gene editing or artificial intelligence or nuclear adoption. pTA helps grow institutional knowledge and expertise about complex topics as well as about public attitudes and concerns salient to those topics at scale. For example, challenges associated with COVID-19 vaccines presented several opportunities to deploy pTA. Public trust of the government’s pandemic response was uneven at best. Many Americans reported specific concerns about receiving a COVID-19 vaccine. Public opinion polls have delivered mixed messages regarding willingness to receive a COVID- 19 vaccine, but polls can overlook other historically significant concerns and socio-political developments in rapidly changing environments. Demands for expediency in vaccine development complicated the situation when normal safeguards and oversights were relaxed. Apparent pressure to deliver a vaccine as soon as possible raised public concern that vaccine safety is not being adequately vetted. Logistical and ethical questions about vaccine rollout were also abound: who should get vaccinated first, at what cost, and alongside what other public health measures? The nation needed a portfolio of differentiated and locally robust strategies for vaccine deployment. pTA would help officials anticipate equity challenges and trust deficits related to vaccine use and inform messaging and means of delivery, helping effective and socially robust rollout strategies for different communities across the country.
pTA is an Established Practice
pTA has a history of use in the European Union and more recently in the United States. Inspired partly by the former U.S. Office of Technology Assessment (OTA), many European nations and the European Parliament operate their own technology assessment (TA) agencies. European TA took a distinctive turn from the OTA in further democratizing science and technology decision-making by developing and implementing a variety of effective and economical practices involving citizen participation (or pTA). Recent European Parliamentary Technology Assessment reports have taken on issues of assistive technologies, future of work, future of mobility, and climate-change innovation.
In the United States, a group of researchers, educators, and policy practitioners established the Expert and Citizen Assessment of Science and Technology (ECAST) network in 2010 to develop a distinctive 21st-century model of TA. Over the course of a decade, ECAST developed an innovative and reflexive participatory technology assessment (pTA) method to support democratic decision-making in different technical, social, and political contexts. After a demonstration project providing citizen input to the United Nations Convention on Biological Diversity in collaboration with the Danish Board of Technology, ECAST, worked with the National Aeronautics and Space Administration (NASA) on the agency’s Asteroid Initiative. NASA-sponsored pTA activities about asteroid missions revealed important concerns about mitigating asteroid impact alongside decision support for specific NASA missions. Public audiences prioritized a U.S. role in planetary defense from asteroid impacts. These results were communicated to NASA administrators and informed the development of NASA’s Planetary Defense Coordination Office, demonstrating how pTA can identify novel public concerns to inform decision making.
This NASA pTA paved the way for pTA projects with the Department of Energy on nuclear-waste disposal and with the National Oceanic and Atmospheric Administration on community resilience. ECAST’s portfolio also includes projects on climate intervention research, the future of automated vehicles, gene editing, clean energy demonstration projects and interim storage of spent nuclear fuel. These and other pTA projects have been supported by more than six million dollars of public and philanthropic funding over the past ten years. Strong funding support in recent years highlights a growing demand for public engagement in science and technology decision-making.
However, the current scale of investment in pTA projects is vastly outstripped by the number of agencies and policy decisions that stand to benefit from pTA and are demanding applications for different use cases from public education, policy decisions, public value mapping and process and institutional innovations. ECAST’s capacity and ability to partner with federal agencies is limited and constrained by existing administrative rules and procedures on the federal side and resources and capacity deficiencies and flexibilities on the network side. Any external entity like ECAST will encounter difficulties in building institutional memory and in developing cooperative-agreement mechanisms across agencies with different missions as well as within agencies with different divisions. Integrating public engagement as a standard component of decision making will require aligning the interests of sponsoring agencies, publics, and pTA practitioners within the context of broad and shifting political environments. An FFRDC office dedicated to pTA would provide the embedded infrastructure, staffing, and processes necessary to achieve these challenging tasks. A dedicated home for pTA within the executive branch would also enable systematic research, evaluation, and training related to pTA methods and practices, as well as better integration of pTA tools into decision making involving public education, research, innovation and policy actions.
Plan of Action
The next administration should support and conduct pTA across the Federal Government by expanding the scope of the Science and Technology Policy Institute (STPI) to include a special unit with a separate operating budget dedicated specifically to pTA. STPI is an existing federally funded research and development center (FFRDC) that already conducts research on emerging technological challenges for the Federal Government. STPI is strategically associated with the White House Office of Science and Technology Policy (OSTP). Integrating pTA across federal agencies aligns with STPI’s mission to provide technical and analytical support to agency sponsors on the assessment of critical and emerging technologies.
A dedicated pTA unit within STPI would (1) provide expertise and resources to conduct pTA for federal agencies and (2) document and archive broader public expertise captured through pTA. Much publicly valuable knowledge generated from one area of S&T is applicable to and usable in other areas. As part of an FFRDC associated with the executive branch, STPI’s pTA unit could collaborate with universities to help disseminate best practices across all executive agencies.
We envision that STPI’s pTA unit would conduct activities related to the general theory and practice of pTA as well as partner with other federal agencies to integrate pTA into projects large and small. Small-scale projects, such as a series of public focus groups, expert consultations, or general topic research could be conducted directly by the pTA unit’s staff. Larger projects, such as a series of in-person or online deliberative engagements, workshops, and subsequent analysis and evaluation, would require additional funding and support from the requesting agencies. The STPI pTA unit could also establish longer-term partnerships with universities and science centers (as in the ECAST network), thereby enabling the federal government to leverage and learn from pTA exercises sponsored by non-federal entities.
The new STPI pTA unit would be funded in part through projects requested by other federal agencies. An agency would fund the pTA unit to design, plan, conduct, assess, and analyze a pTA effort on a project relevant to the agency. This model would enable the unit to distribute costs across the executive branch and would ensure that the unit has access to subject-matter experts (i.e., agency staff) needed to conduct an informed pTA effort. Housing the unit within STPI would contribute to OSTP’s larger portfolio of science and technology policy analysis, open innovation and citizen science, and a robust civic infrastructure.
Cost and Capacities
Adding a pTA unit to STPI would increase federal capacity to conduct pTA, utilizing existing pathways and budget lines to support additional staff and infrastructure for pTA capabilities. Establishing a semi-independent office for pTA within STPI would make it possible for the executive branch to share support staff and other costs. We anticipate that $3.5–5 million per year would be needed to support the core team of researchers, practitioners, leadership, small-scale projects, and operations within STPI for the pTA unit. This funding would require congressional approval.
The STPI pTA unit and its staff would be dedicated to housing and maintaining a critical infrastructure for pTA projects, including practical know-how, robust relationships with partner organizations (e.g., science centers, museums, or other public venues for hosting deliberative pTA forums), and analytic capabilities. This unit would not wholly be responsible for any given pTA effort. Rather, sponsoring agencies should provide resources and direction to support individual pTA projects.
We expect that the STPI pTA unit would be able to conduct two or three pTA projects per year initially. Capacity and agility of the unit would expand as time went on to meet the growth and demands from the federal agencies. In the fifth year of the unit (the typical length of an FFRDC contract), the presidential administration should consider whether there is sufficient agency demand for pTA—and whether the STPI pTA unit has sufficiently demonstrated proof-of-concept—to merit establishment of a new and independent FFRDC or other government entity fully dedicated to pTA.
Operations
The process for initiating, implementing and finalizing a pTA project would resemble the following:
Pre:
- Agency approaches the pTA unit with interest in conducting pTA for agency assessment and decision making for a particular subject.
- pTA unit assists the agency in developing questions appropriate for pTA. This process involves input from agency decision makers and experts as well as external stakeholders.
- A Memorandum of understanding/agreement (MOU/MOA) is created, laying out the scope of the pTA effort.
During:
- pTA unit and agency convene expert and/or public workshops (as appropriate) to inform pTA activities.
- pTA unit and agency create, test, and evaluate prototype pTA activities (see FAQs below for more details on evaluation).
- pTA unit and agency work with a network of pTA host institutions (e.g, science centers, universities, nonprofit organizations, etc.) to coordinate pTA forums.
- pTA unit oversees pTA forums.
Post:
- pTA unit collects, assesses, and analyzes pTA forum results with iterative input and analysis from the hosting agency.
- pTA unit works with stakeholders to share and finalize pTA reports on the subject, as well as a dissemination plan for sharing results with stakeholder groups.
Conclusion
Participatory Technology Assessment (pTA) is an established suite of tools and processes for eliciting and documenting informed public values and opinions to contribute to decision making around complex issues at the intersections of science, technology, and society.
However, its creative adaptation and innovative use by federal agencies in recent years demonstrate their utility beyond providing decision support: from increasing scientific literacy and social acceptability to diffusing tensions and improving mutual trust. By creating capacity for pTA within STPI, the incoming administration will bolster its ability to address longstanding and emerging issues that lie at the intersection of scientific progress and societal well-being, where progress depends on aligning scientific, market and public values. Such capacity and capabilities will be crucial to improving the legitimacy, transparency, and accountability of decisions regarding how we navigate and tackle the most intractable problems facing our society, now and for years to come.
This action-ready policy memo is part of Day One 2025 — our effort to bring forward bold policy ideas, grounded in science and evidence, that can tackle the country’s biggest challenges and bring us closer to the prosperous, equitable and safe future that we all hope for whoever takes office in 2025 and beyond.
PLEASE NOTE (February 2025): Since publication several government websites have been taken offline. We apologize for any broken links to once accessible public data.
Experts can help map potential policy and R&D options and their implications. However, there will always be an element of judgment when it comes to deciding among options. This stage is often more driven by ethical and social concerns than by technical assessments. For instance, leaders may need to figure out a fair and just process to govern hazardous-waste disposal, or weigh the implications of using genetically modified organisms to control diseases, or siting clean energy research and demonstration projects in resistant or disadvantaged communities. Involving the public in decision-making can help counter challenges associated with expert judgment (for example, “groupthink”) while bringing in perspectives, values, and considerations that experts may overlook or discount.
pTA incorporates a variety of measures to inform discussion, such as background materials distributed to participants and multimedia tools to provide relevant information about the issue. The content of background materials is developed by experts and stakeholders prior to a pTA event to give the public the information they need to thoughtfully engage with the topic at hand. Evaluation tools, such as those from the informal science-education community, can be used to assess how effective background materials are at preparing the public for an informed discussion, and to identify ineffective materials that may need revision or supplementation. Evaluations of several past pTA efforts have 1) shown consistent learning among public participants and 2) have documented robust processes for the creation, testing, and refinement of pTA activities that foster informed discussions among pTA participants.
pTA can result in products and information, such as reports and data on public values, that are relevant and useful for the communication missions of agencies. However, pTA should avoid becoming a tool for strategic communications or a procedural “checkbox” activity for public engagement. Locating the Federal Government’s dedicated pTA unit within an FFRDC will ensure that pTA is informed by and accountable to a broader community of pTA experts and stakeholders who are independent of any mission agency.
The work of universities, science centers, and nonpartisan think tanks have greatly expanded the tools and approaches available for using pTA to inform decision-making. Many past and current pTA efforts have been driven by such nongovernmental institutions, and have proven agile, collaborative, and low cost. These efforts, while successful, have limited or diffuse ties to federal decision making.
Embedding pTA within the federal government would help agencies overcome the opportunity and time cost of integrating public input into tight decision-making timelines. ECAST’s work with federal agencies has shown the need for a stable bureaucratic infrastructure surrounding pTA at the federal level to build organizational memory, create a federal community of practice, and productively institutionalize pTA into federal decision-making.
Importantly, pTA is a nonpartisan method that can help reduce tensions and find shared values. Involving a diversity of perspectives through pTA engagements can help stakeholders move beyond impasse and conflict. pTA engagements emphasize recruiting and involving Americans from all walks of life, including those historically excluded from policymaking.
Currently, the Government Accountability Office’s Science, Technology Assessment, and Analytics team (STAA) conducts technology assessments for Congress. Technology Assessment (TA) is designed to enhance understanding of the implications of new technologies or existing S&T issues. The STAA certainly has the capacity to undertake pTA studies on key S&T issues if and when requested by Congress. However, the distinctive form of pTA developed by ECAST and exemplified in ECAST’s work with NASA, NOAA, and DOE follows a knowledge co- production model in which agency program managers work with pTA practitioners to co-design, co-develop, and integrate pTA into their decision-making processes. STAA, as a component of the legislative branch, is not well positioned to work alongside executive agencies in this way. The proposed pTA unit within STPI would make the proven ECAST model available to all executive agencies, nicely complementing the analytical TA capacity that STAA offers the federal legislature.
Executive orders could support one-off pTA projects and require agencies to conduct pTA. However, establishing a pTA unit within an FFRDC like STPI would provide additional benefits that would lead to a more robust pTA capacity.
FFRDCs are a special class of research institutions owned by the federal government but operated by contractors, including universities, nonprofits, and industrial firms. The primary purpose of FFRDCs is to pursue research and development that cannot be effectively provided by the government or other sectors operating on their own. FFRDCs also enable the government to recruit and retain diverse experts without government hiring and pay constraints, providing the government with a specialized, agile workforce to respond to agency needs and societal challenges.
Creating a pTA unit in an FFRDC would provide an institutional home for general pTA know-how and capacity: a resource that all agencies could tap into. The pTA unit would be staffed by a small but highly-trained staff who are well-versed in the knowledge and practice of pTA. The pTA unit would not preclude individual agencies from undertaking pTA on their own, but would provide a “help center” to help agencies figure out where to start and how to overcome roadblocks. pTA unit staff could also offer workshops and other opportunities to help train personnel in other agencies on ways to incorporate the public perspective into their activities.
Other potential homes for a dedicated federal pTA unit include the Government Accountability Office (GAO) or the National Academies of Sciences, Engineering, and Medicine. However, GAO’s association with Congress would weaken the unit’s connections to agencies. The National Academies historically conduct assessments driven purely by expert consensus, which may compromise the ability of National Academies-hosted pTA to include and/or emphasize broader public values.
Evaluating a pTA effort means answering four questions:
First, did the pTA effort engage a diverse public not otherwise engaged in S&T policy formulation? pTA practitioners generally do not seek statistically representative samples of participants (unlike, for instance, practitioners of mass opinion polling). Instead, pTA practitioners focus on including a diverse group of participants, with particular attention paid to groups who are generally not engaged in S&T policy formulation.
Second, was the pTA process informed and deliberative? This question is generally answered through strategies borrowed from the informal science-learning community, such as “pre- and post-“ surveys of self-reported learning. Qualitative analysis of the participant responses and discussions can evaluate if and how background information was used in pTA exercises. Involving decision makers and stakeholders in the evaluation process—for example, through sharing initial evaluation results—helps build the credibility of participant responses, particularly when decision makers or agencies are skeptical of the ability of lay citizens to provide informed opinions.
Third, did pTA generate useful and actionable outputs for the agency and, if applicable, stakeholders? pTA practitioners use qualitative tools for assessing public opinions and values alongside quantitative tools, such as surveys. A combination of qualitative and quantitative analysis helps to evaluate not just what public participants prefer regarding a given issue but why they hold that preference and how they justify those preferences. To ensure such information is useful to agencies and decision makers, pTA practitioners involve decision makers at various points in the analysis process (for example, to probe participant responses regarding a particular concern). Interviews with decision makers and other stakeholders can also assess the utility of pTA results.
Fourth, what impact did pTA have on participants, decisions and decision-making processes, decision makers, and organizational culture? This question can be answered through interviews with decision makers and stakeholders, surveys of pTA participants, and impact assessments.
Evaluation of a pTA unit within an existing FFRDC would likely involve similar questions as above: questions focused on the impact of the unit on decisions, decision-making processes, and the culture and attitudes of agency staff who worked with the pTA unit. An external evaluator, such as the Government Accountability Office or the National Academies of Sciences, could be tasked with carrying out such an evaluation.
pTA results and processes should typically be made public as long as few risks are posed to pTA participants (in line with federal regulations protecting research participants). Publishing results and processes ensures that stakeholders, other members of government (e.g., Congress), and broader audiences can view and interpret the public values explored during a pTA effort. Further, making results and processes publicly available serves as a form of accountability, ensuring that pTA efforts are high quality.
An Innovation Agenda for Addiction: Breakthrough Medicines That Scale
The federal government should expand the FDA’s priority review voucher program (PRV) and provide market exclusivity advantages to encourage the development of medications for addiction.
Taken together, substance use disorders (alcohol, cigarettes, and other drugs) cause more deaths in the U.S. every year than cancer or heart disease and cause devastating downstream social harms. Despite this, only 3% of eligible patients received substance use disorder (SUD) medication, a result of low uptake and efficacy of existing medications and a lack of options for patients addicted to stimulants. This is due to a near-total absence of pharmaceutical research and development activity. To make population level impact to reduce harms from opioids, methamphetamine, cocaine, alcohol, and cigarettes, we must address the broken market dynamics in addiction medicine.
The PRV program should be expanded to cover opioid use disorder, alcohol use disorder, stimulant use disorder, and smoking. In addition, drugs that are approved for these SUD indications should have extended exclusivity and sponsors that develop these medications should receive vouchers to extend exclusivity for other medications.
Challenge and Opportunity
Addiction policy efforts on both the left and the right have struggled. Despite substantial progress reducing smoking, 29 million Americans still smoke cigarettes and feel unable to quit and 480,000 Americans die each year from smoking. While overdose deaths from opioids, cocaine, and methamphetamine have fallen slightly from their peak in 2022, they are still near record highs, three times higher than 20 years ago. Alcohol deaths per capita have doubled since 1999.
Roughly 60% of all crimes and 65% of violent crimes are related to drugs or alcohol; and the opioid crisis alone costs the United States $1.5 trillion a year. Progress in reducing addiction is held back because people with a substance use disorder take medication. This low uptake has multiple causes: in opiate use disorder, uptake is persistently low despite recent relaxations of prescription rules, with patients reporting a variety of reasons for refusal; treatments for alcohol use disorder have modest effects; and there are no approved treatments for stimulant use disorder. Only three percent take SUD medications, as shown in figure 1 below [link to image]. In brief, only 2% of those suffering alcohol use disorder, 13% of those with opiate use disorder, 2% of smokers, and approximately 0% of illicit stimulant users are receiving medication, giving a weighted average of about 3%.
There has been rapid innovation in the illicit market as synthetic opioids and expanded meth production have lowered price and increased strength and availability. Meanwhile, there has been virtually no innovation in medicines to prevent and treat addiction. The last significant FDA approval for opioid use disorder was buprenorphine in 2002; progress since then has been minimal, with new formulations or dosing of old medications. For alcohol use disorder, the most recent was acamprosate in 2004 (and it is rarely prescribed due to limited efficacy and three times a day dosing).
None of the ten largest pharmaceutical companies have active addiction medicine programs or drug candidates, and the pharmaceutical industry as a whole has only pursued minimal drug development. According to the trade association BIO, “Venture investment into companies with novel addiction drug programs over the last 10 years is estimated at $130M, 270 times less than oncology.”
There are promising addiction drug candidates being studied by academics but without industry support they will never become medicines. If pharmaceutical companies spent just 10% of what they spend on obesity therapies, we might quickly make progress.
For example, GLP-1 medicines like Ozempic and Mounjaro have strong anti-addictive effects across substances. Randomized trials and real-world patient health record studies show dramatic drops in consumption of drugs and alcohol for patients taking a GLP-1. Many addiction scientists now consider these compounds to be the biggest breakthrough in decades. However, Novo Nordisk and Eli Lilly, who own the drugs currently in the market, do not plan to run phase 3 addiction trials on them, due to fear of adverse events in substance use disorder populations. The result is that a huge medical opportunity is stuck in limbo indefinitely. Fortunately, Lilly has recently signaled that they will run trials on related compounds, but remain years from approval.
Conversations with industry leaders make clear that large pharmas avoid SUD indications for several reasons. First, their upside appears limited, since current SUD medications have modest sales. Second, like other psychiatric disorders, the problem is challenging given the range and complexity of neurological targets and the logistical challenges of recruiting people with substance use disorder as participants. Finally, companies face downside reputational and regulatory risk if participants, who face high baseline rates of death from overdose regardless, were to die in trials. In the case of Ozempic and Mounjaro, sponsors face an obstacle some have termed the “problem of new uses” – clinical trials of an already lucrative drug for a new indication carry downside risk if new side effects or adverse events are reported.
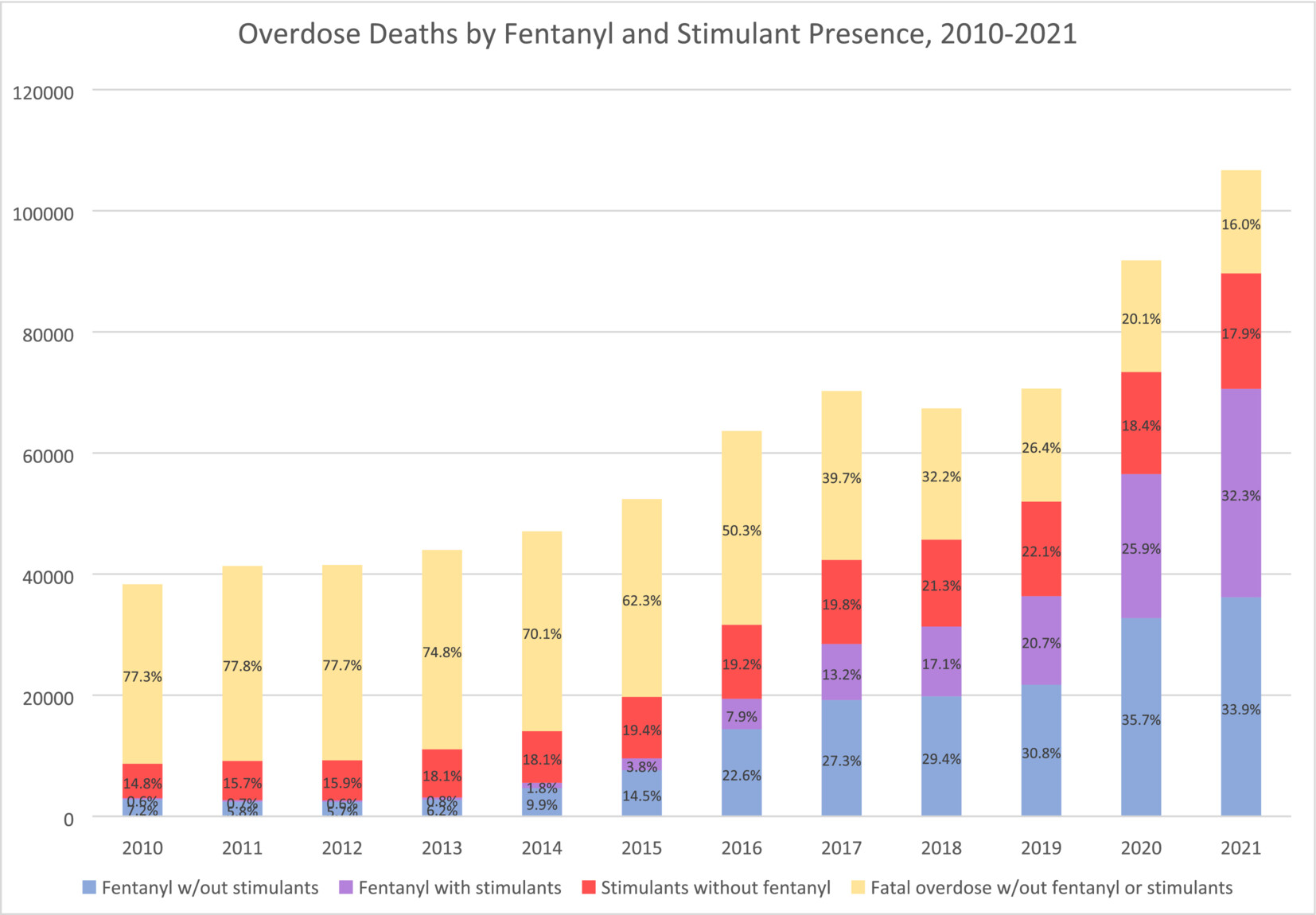
Image from Charting the fourth wave, based on CDC data
Plan of Action
Market Shaping Interventions
Recommendation 1. Expand the FDA priority review voucher (PRV) program to include addiction medicine indications.
The FDA priority review voucher (PRV) program incentivizes development of drugs for rare pediatric and infectious diseases by rewarding companies who get drugs approved with a transferable voucher that accelerates FDA approval. These vouchers are currently selling for an average of $100M. The PRV program doesn’t cost the government any money but it makes drug development in the designated categories much more lucrative. The PRV program has proven very successful, leading to a surge in approvals of medications.
As a neglected market with urgent unmet medical and public health needs, and which also promises to benefit the broader public by reducing the negative externalities of addiction, addiction medicine is a perfect fit for the PRV program. Doing so could transform the broken market dynamics of the field. The advantage of the PRV program is that it does not require substantial new congressional appropriations, though it will require Congress giving the FDA authority to expand the PRV program, as it has done previously to add other disease areas.
Recommendation 2. Extend exclusivity for addiction medicines and incentivize pursuit of new indications
Market exclusivity is a primary driver of pharmaceutical industry revenue. Extending exclusivities would have a very large effect on industry behavior and is needed to create sufficient incentives. The duration of exclusivity for alcohol use disorder, opioid use disorder, stimulant use disorder, and smoking cessation indications should be extended along with other incentives.
- Addiction medicine indications should receive an additional two years of exclusivity for biologics and three years for small molecules.
- Companies that achieve an indication for a substance use disorder for a medication that represents a significant advance would receive an exclusivity voucher that can be transferred to another medication. For 2nd, 3rd, and 4th SUD indications with the same compound, companies would be granted a shorter duration exclusivity voucher. Durations would be tiered, as described in this proposal from Duke, to balance public interest and reward levels.
- FDA should provide increased consideration for addiction medicines for breakthrough, fast track, and priority review designations, as well as accelerate meeting schedules, all of which substantially reduce development expenses.
For precedent, there are already a number of FDA programs that extend medication exclusivity, including ‘orphan drug exclusivity’ and the qualified infectious disease product (QIDP) program. Like rare diseases and antibiotics, addiction is a market that requires incentives to function effectively. In addition, successful treatments, given the negative externalities of addiction, have public benefit beyond the direct medical impact, and deserve additional public incentives.
Recommendation 3. Modernize FDA Standards of Efficacy for Substance Use Disorder Trials
A significant barrier to pharmaceutical innovation in SUDs is outdated or unpredictable efficacy standards sometimes set by the FDA for clinical trials. Efficacy expectations for substance use disorder indications are often rooted in abstinence-only and other binary measure orientations that the scientific and medical community has moved past when evaluating substance use disorder harms.
This article in the American Journal of Drug and Alcohol Abuse demonstrates that binary outcome measures like ‘number of heavy drinking days’ (NHDD) can underestimate the efficacy of treatments. This recent report from NIAAA on alcohol trial endpoints recommends a shift away from abstinence-based endpoints and towards more meaningful consumption-based endpoints. This approach should be adopted by the FDA for all SUD treatments, not just alcohol.
There are some indications that the FDA has begun modernizing their approach. This recent paper from NIH and FDA on smoking cessation therapies provides updated guidance that moves in the right direction.
More broadly, the FDA should work to adopt endpoints and standards of efficacy that mirror standards in other disease areas. This shift is best achieved through new guidance or statements issued by the FDA, which would offer positive assurance to pharmaceutical companies that they have achievable paths to approval. Predictability throughout the medication development life cycle is absolutely essential for companies considering investment.
Congress should include statements in upcoming appropriations and authorizations that state:
- The FDA should adopt non-binary standards of efficacy for addiction treatments that are aligned with standards for other common disorders and the FDA shall, within 12 months, report on the standards employed for substance use disorder relative to other prevalent chronic conditions and report steps to eliminate disparities in evidentiary standards and issue new guidance on the subject.
- The FDA should publish clear guidance on endpoints across SUDs to support planning among pharmaceutical companies considering work in this field.
Conclusion
Sustained focus and investment in diabetes and heart disease treatments has enabled medical breakthroughs. Addiction medicine, by contrast, has been largely stagnant for decades. Stimulating private-sector interest in addiction medicine through regulatory and exclusivity incentives, as well as modernized efficacy standards, is essential for disrupting the status quo. Breakthroughs in addiction medicine could save hundreds of thousands of lives in the US and provide long-term relief for one of our most intractable social problems. Given the negative externalities of addiction, this would also have enormous benefits for society at large, reducing crime and intergenerational trauma and saving money on social services and law enforcement.
This action-ready policy memo is part of Day One 2025 — our effort to bring forward bold policy ideas, grounded in science and evidence, that can tackle the country’s biggest challenges and bring us closer to the prosperous, equitable and safe future that we all hope for whoever takes office in 2025 and beyond.
PLEASE NOTE (February 2025): Since publication several government websites have been taken offline. We apologize for any broken links to once accessible public data.
Per author conversations with industry leaders, private sector interest in SUD medication development is limited for the following reasons:
- The upside of pursuing SUD indications appears limited, since current SUD medications, which are generally targeted for specific substances, have modest sales.
- Even with preliminary evidence that GLP-1 drugs may be efficacious for some SUD indications (e.g, alcohol, opiates, and tobacco), companies are reluctant to pursue label expansion for SUD. As described previously, with already lucrative drugs, companies face a downside risk (termed the “problem of new uses”) from running large clinical trials, and possibly uncovering new side effects or incurring random adverse events which could harm reputation and existing markets.
- In the specific case of SUD, this downside risk might be especially large, since people with substance use disorder have high baseline rates of overdose and death.
Moreover, there is an argument that a treatment for SUD is a public good, to the degree that it ameliorates the negative externalities of addiction – increasing the case for more public-sector incentives for SUD treatment. The end result is that medical treatments for SUD are stuck in an indefinite limbo, with private-sector interest in SUD, as documented previously, being very low.
The current lack of effective and widely used SUD medications is disheartening, but this is in the context of private sector disinterest and scant funding. Even modest successes in SUD treatment have the potential to kickstart an innovation loop, akin to the rush of biotech companies hastening to enter the obesity treatment field. Prior to the success of the GLP-1 drugs, obesity treatment had been moribund, and viewed pessimistically in light of drugs that had limited efficacy or had been withdrawn for side effects like suicidality or cardiovascular issues.
An SUD success like GLP-1 for obesity has the potential to kindle a similar rush of interest; the challenge is the initiation of that cascade. Given the very low levels of investment in SUD treatments, there is potential low-hanging fruit that, given sufficient funding, could be trialed and deployed.
There has been rapid innovation in the field of addiction, but it’s been happening on the wrong side: addiction-inducing technologies are becoming more powerful, while SUD treatments have largely stagnated. This innovation is most evident in synthetic opioids and methamphetamine.
Compared to heroin, fentanyl is about 25x stronger (on a per-weight basis), and hence, much easier to smuggle. As the Commission on Combating Synthetic Opioid Trafficking put it:
Single-digit metric tonnage of pure fentanyl is not a large amount and could easily fit into a shipping container or a truck trailer, which seriously challenges interdiction…Perhaps as much as 5 MT [metric tons] of pure fentanyl would be needed to satisfy the entire annual U.S. consumption for illegally supplied opioids.
Moreover, as a recent Scientific American article documented, innovations in fentanyl production, including the use of safer precursors and methods that don’t require sophisticated equipment, mean that fentanyl production is now decentralized, and resistant to attempts by law enforcement to shut it down.
As fentanyl has come to dominate the opioid supply over the past 10 years, overdose deaths have risen dramatically. New synthetic opioids and non-opioids like xylazine are also becoming common.
At the same time, due to advances in production techniques in Mexico, methamphetamine production has skyrocketed in recent decades while purity has improved. Worst of all, unlike heroin, fentanyl is easily combined with meth and cocaine in pills and powder.
The DEA has highlighted the presence of “super labs” in Mexico capable of producing hundreds of pounds of meth per batch.
Together, these three innovations (fentanyl, cheap meth, and new combinations) have led to a 400% increase in overdose deaths in the past 20 years. Without equally powerful innovations to reduce addiction rates, we will never make long-term and sustainable progress.
A Dose Of Reality: Underscoring The Fatal Consequences Of The Opioid Epidemic
The opioid epidemic is a public health and safety emergency that is killing thousands and destroying the quality of life for hundreds of thousands of Americans and those who care about them. Fentanyl and other opioids affect all age ranges, ethnicities, and communities, including our most vulnerable population, children. Producing fentanyl is increasingly cheap, costing pennies for a fatal dose, with the opioid intentionally or unintentionally mixed with common illicit street drugs and pressed into counterfeit pills. Fentanyl is odorless and tasteless, making it nearly untraceable when mixed with other drugs. Extremely small doses of fentanyl, roughly equivalent to a few grains of salt, can be fatal, while carfentanil, a large animal tranquilizer, is 100 times more potent than fentanyl and fatal at an even smaller amount.
The Biden-Harris Administration should do even more to fund opioid-related prevention, treatment, eradication, and interdiction efforts to save lives in the United States. The 2022 Executive Order to Address the Opioid Epidemic and Support Recovery awarded $1.5 billion to states and territories to expand treatment access, enhance services in rural communities, and fund law enforcement efforts. In his 2023 State of the Union address, President Biden highlighted reducing opioid overdoses as part of his bipartisan Unity Agenda, pledging to disrupt trafficking and sales of fentanyl and focus on prevention and harm reduction. Despite extensive funding, opioid-related overdoses have not significantly decreased, showing that a different strategy is needed to save lives.
Opioid-related deaths have been estimated cost the U.S. nearly $4 trillion over the past seven years—not including the human aspect of the deaths. The cost of fatal overdoses was determined to be $550 billion in 2017. The cost of the opioid epidemic in 2020 alone was an estimated $1.5 trillion, up 37% from 2017. About two-thirds of the cost was due to the value of lives lost and opioid use disorder, with $35 billion spent on healthcare and opioid-related treatments and about $15 billion spent on criminal justice involvement. In 2017, per capita costs of opioid use disorder and opioid toxicity-related deaths were as high as $7247, with the cost per case of opioid use disorder over $221,000. With inflation in November 2023 at $1.26 compared to $1 in 2017, not including increases in healthcare costs and the significant increase in drug toxicity-related deaths, the total rate of $693 billion is likely significantly understated for fatal overdoses in 2023. Even with extensive funding, opioid-related deaths continue to rise.
With fatal opioid-related deaths being underreported, the Centers for Disease Control and Prevention (CDC) must take a primary role in real-time surveillance of opioid-related fatal and non-fatal overdoses by funding expanded toxicology testing, training first responder and medicolegal professionals, and ensuring compliance with data submission. The Department of Justice (DOJ) should support enforcement efforts to reduce drug toxicity-related morbidity and mortality, with the Department of Homeland Security (DHS) and the Department of the Treasury (TREAS) assisting with enforcement and sanctions, to prevent future overdoses. Key recommendations for reducing opioid-related morbidity and mortality include:
- Funding research to determine the efficacy of current efforts in opioid misuse reduction and prevention.
- Modernizing data systems and surveillance to provide real-time information.
- Increasing overdose awareness, prevention education, and availability of naloxone.
- Improve training of first responders and medicolegal death investigators.
- Funding rapid and thorough toxicology testing in emergency departments and coroner/medical examiner agencies.
- Enhancing prevention and enforcement efforts.
Challenge and Opportunity
Opioids are a class of drugs, including pain relievers that can be illegally prescribed and the illicit drug heroin. There are three defined waves of the opioid crisis, starting in the early 1990s as physicians increasingly prescribed opioids for pain control. The uptick in prescriptions stemmed from pharmaceutical companies promising physicians that these medications had low addiction rates and medical professionals adding pain levels being added to objective vital signs for treatment. From 1999 to 2010, prescription opioid sales quadrupled—and opioid-related deaths doubled. During this time frame when the relationship between drug abuse and misuse was linked to opioids, a significant push was made to limit physicians from prescribing opioids. This contributed to the second wave of the epidemic, when heroin abuse increased as former opioid patients sought relief. Heroin-related deaths increased 286% from 2002 to 2013, with about 80% of heroin users acknowledging that they misused prescription opioids before using heroin. The third wave of the opioid crisis came in 2013 with an increase in illegally manufactured fentanyl, a synthetic opioid used to treat severe pain that is up to 100 times stronger than morphine, and carfentanil, which is 100 times more potent than fentanyl.
In 2022, nearly 110,000 people in the United States died from drug toxicity, with about 75% of the deaths involving opioids. In 2021, six times as many people died from drug overdoses as in 1999, with a 16% increase from 2020 to 2021 alone. While heroin-related deaths decreased by over 30% from 2020 to 2021, opioid-related deaths increased by 15%, with synthetic opioid-involved deaths like fentanyl increasing by over 22%. Over 700,000 people have died of opioid-related drug toxicity since 1999, and since 2021 45 people have died every day from a prescription opioid overdose. Opioid-related deaths have increased tenfold since 1999, with no signs of slowing down. The District of Columbia declared a public emergency in November 2023 to draw more attention to the opioid crisis.
In 2023, we are at the precipice of the fourth wave of the crisis, as synthetic opioids like fentanyl are combined with a stimulant, commonly methamphetamine. Speedballs have been common for decades, using stimulants to counterbalance the fatigue that occurs with opiates. The fatal combination of fentanyl and a stimulant was responsible for just 0.6% of overdose deaths in 2010 but 32.3% of opioid deaths in 2021, an over fifty-fold increase in 12 years. Fentanyl, originally used in end-of-life and cancer care, is commonly manufactured in Mexico with precursor chemicals from China. Fentanyl is also commonly added to pressed pills made to look like legitimate prescription medications. In the first nine months of 2023, the Drug Enforcement Agency (DEA) seized over 62 million counterfeit pills and nearly five tons of powdered fentanyl, which equates to over 287 million fatal doses. These staggering seizure numbers do not include local law enforcement efforts, with the New York City Police Department recovering 13 kilos of fentanyl in the Bronx, enough powder to kill 6.5 million people.
The ease of creating and trafficking fentanyl and similar opioids has led to an epidemic in the United States. Currently, fentanyl can be made for pennies and sold for as little as 40 cents in Washington State. The ease of availability has led to deaths in our most vulnerable population—children. Between June and September 2023, there were three fatal overdoses of children five years and younger in Portland, OR. In a high-profile case in New York City, investigators found a kilogram of fentanyl powder in a day care facility after a 1-year-old died and three others became critically ill.
The Biden Administration has responding to the crisis in part by placing sanctions against and indicting executives in Chinese companies for manufacturing and distributing precursor chemicals, which are commonly sold to Mexican drug cartels to create fentanyl. The drug is then trafficked into the United States for sale and use. There are also concerns about fentanyl being used as a weapon of mass destruction, similar to the anthrax concerns in the early 2000s.
The daily concerns of opioid overdoses have plagued public health and law enforcement professionals for years. In Seattle, WA, alone, there are 15 non-fatal overdoses daily, straining the emergency medical systems. There were nearly 5,000 non-fatal overdoses in the first seven months of 2023 in King County, WA, an increase of 70% compared to 2022. In a landmark decision, in March 2023 the Food and Drug Administration (FDA) approved naloxone, a drug to reverse the effects of opioid overdoses, as an over-the-counter nasal spray in an attempt to reduce overdose deaths. Naloxone nasal spray was initially approved for prescription use only in 2015 , significantly limiting access to first responders and available to high-risk patients when prescribed opioids. In New York, physicians have been required to prescribe naloxone to patients at risk of overdose since 2022. Although naloxone is now available without a prescription, access is still limited by price, with one dose costing as much as $65, and some people requiring more than one dose to reverse the overdose. Citing budget concerns, Governor Newsom vetoed California’s proposed AB 1060, which would have limited the cost of naloxone to $10 per dose. Fentanyl testing strips that can be used to test substances for the presence of fentanyl before use show promise in preventing unwanted fentanyl-adulterated overdoses. The Expanding Nationwide Access to Test Strips Act, which was introduced to the Senate in July 2023, would decriminalize the testing strips as an inexpensive way to reduce overdose while following evidence-based harm-reduction theories.
Illicit drugs are also one of the top threats to national security. Law enforcement agencies are dealing with a triple epidemic of gun violence, the opioid crisis, and critical staffing levels. Crime prevention is tied directly to increased police staffing, with lower staffing limiting crime control tactics, such as using interagency task forces, to focus on a specific crime problem. Police are at the forefront of the opioid crisis, expected to provide an emergency response to potential overdoses and ensure public safety while disrupting and investigating drug-related crimes. Phoenix Police Department seized over 500,000 fentanyl pills in June 2023 as part of Operation Summer Shield, showing law enforcement’s central role in fighting the opioid crisis. DHS created a comprehensive interdiction plan to reduce the national and international supply of opioids, working with the private sector to decrease drugs brought into the United States and increasing task forces to focus on drug traffickers.
Prosecutors are starting to charge drug dealers and parents of children exposed to fentanyl in their residences in fatal overdose cases. In an unprecedented action, Attorney General Merrick Garland recently charged Mexican cartel members with trafficking fentanyl and indicting Chinese companies and their executives for creating and selling precursor chemicals. In November 2023, sanctions were placed against the Sinaloa cartel and four firms from Mexico suspected of drug trafficking to the United States, removing their ability to legally access the American banking system. Despite this work, criminal justice-related efforts alone are not reducing overdoses and deaths, showing a need for a multifaceted approach to save lives.
While these numbers of opioid overdoses are appalling, they are likely underreported. Accurate reporting of fatal overdoses varies dramatically across the country, with the lack of training of medicolegal death investigators to recognize potential drug toxicity-related deaths, coupled with the shortage of forensic pathologists and the high costs of toxicology testing, leading to inaccurate cause of death information. The data ecosystem is changing, with agencies and their valuable data remaining disjointed and unable to communicate across systems. A new model could be found in the CDC’s Data Modernization Initiative, which tracked millions of COVID-19 cases across all states and districts, including data from emergency departments and medicolegal offices. This robust initiative to modernize data transfer and accessibility could be transformative for public health. The electronic case reporting system and strong surveillance systems that are now in place can be used for other public health outbreaks, although they have not been institutionalized for the opioid epidemic.
Toxicology testing can take upwards of 8–10 weeks to receive, then weeks more for interpretation and final reporting of the cause of death. The CDC’s State Unintentional Drug Overdose Reporting System receives data from 47 states from death certificates and coroner/medical examiner reports. Even with the CDC’s extensive efforts, the data-sharing is voluntary, and submission is rarely timely enough for tracking real-time outbreaks of overdoses and newly emerging drugs. The increase of novel psychoactive substances, including the addition of the animal tranquilizer xylazineto other drugs, is commonly not included in toxicology panels, leaving early fatal drug interactions undetected and slowing notification of emerging drugs regionally. The data from medicolegal reports is extremely valuable for interdisciplinary overdose fatality review teams at the regional level that bring together healthcare, social services, criminal justice, and medicolegal personnel to review deaths and determine potential intervention points. Overdose fatality review teams can use the data to inform prevention efforts, as has been successful with infant sleeping position recommendations formed through infant mortality review teams.
Plan of Action
Reducing opioid misuse and saving lives requires a multi-stage, multi-agency approach. This includes expanding real-time opioid surveillance efforts; funding for overdose awareness, prevention, and education; and improved training of first responders and medicolegal personnel on recognizing, responding to, and reporting overdoses. Nationwide, improved toxicology testing and reporting is essential for accurate reporting of overdose-involved drugs and determining the efficacy of efforts to combat the opioid epidemic.
Recommendation 1. Fund research to determine the efficacy of current efforts in opioid misuse reduction and prevention.
DOJ should provide grant funding for researchers to outline all known current efforts of opioid misuse reduction and prevention by law enforcement, public health, community programs, and other agencies. The efforts, including the use of suboxone and methadone, should be evaluated to determine if they follow evidence-based practices, how the programs are funded, and their known effect on the community. The findings should be shared widely and without paywalls with practitioners, researchers, and government agencies to hone their future work to known successful efforts and to be used as a foundation for future evidence-based, innovative program implementation.
Recommendation 2. Modernize data systems and surveillance to provide real-time information.
City, county, regional, and state first responder agencies work across different platforms, as do social service agencies, hospitals, private physicians, clinics, and medicolegal offices. A single fatal drug toxicity-related death has associated reports from a law enforcement officer, fire department personnel, emergency medical services, an emergency department, and a medicolegal agency. Additional reports and information are sought from hospitals and clinics, prior treating clinicians, and social service agencies. Even if all of these reports can be obtained, data received and reviewed is not real-time and not accessible across all of the systems.
Medicolegal agencies are arguably the most underprepared for data and surveillance modernization. Only 43% of medicolegal agencies had a computerized case management system in 2018, which was an increase from 31% in 2004. Outside of county or state property, only 75% of medicolegal personnel had internet access from personal devices. The lack of computerized case management systems and limited access to the internet can greatly hinder case reporting and providing timely information to public health and other reporting agencies.
With the availability and use of naloxone by private persons, the Public Naloxone Administration Dashboard from the National EMS Information System (NEMSIS) should be supported and expanded to include community member administration of naloxone. The emergency medical services data can be aligned with the anonymous upload of when, where, and basic demographics for the recipient of naloxone, which can also be made accessible to emergency departments and medicolegal death investigation agencies. While the database likely will not be used for all naloxone administrations, it can provide hot spot information and notify social services of potential areas for intervention and assistance. The database should be tied to the first responder/hospital/medicolegal database to assist in robust surveillance of the opioid epidemic.
Recommendation 3. Increase overdose awareness, prevention education, and availability of naloxone.
Awareness of the likelihood of poisoning and potential death from the use of fentanyl or counterfeit pills is key in prevention. The DEA declared August 21 National Fentanyl Prevention and Awareness Day to increase knowledge of the dangers of fentanyl, with the Senate adopting a resolution to formally recognize the day in 2023. Many states have opioid and fentanyl prevention tactics on their public health websites, and the CDC has educational campaigns designed to reach young adults, though the education needs to be specifically sought out. Funding should be made available to community organizations and city/county governments to create public awareness campaigns about fentanyl and opioid usage, including billboards, television and streaming ads, and highly visible spaces like buses and grocery carts.
ED allows evidence-based prevention programs in school settings to assist in reducing risk factors associated with drug use and misuse. The San Diego Board of Supervisors approved a proposal to add education focused on fentanyl awareness after 12 juveniles died of fentanyl toxicity in 2021. The district attorney supported the education and sought funding to sponsor drug and alcohol training on school campuses. Schools in Arlington, VA, note the rise in overdoses but recognize that preventative education, when present, is insufficient. ED should create prevention programs at grade-appropriate levels that can be adapted for use in classrooms nationwide.
With the legalization of over-the-counter naloxone, funding is needed to provide subsidized or free access to this life-saving medication. Powerful fentanyl analogs require higher doses of naloxone to reverse the toxicity, commonly requiring multiple naloxone administrations, which may not be available to an intervening community member. The State of Washington’s Department of Public Health offers free naloxone kits by mail and at certain pharmacies and community organizations, while Santa Clara University in California has a vending machine that distributes naloxone for free. While naloxone reverses the effects of opioids for a short period, once it wears off, there is a risk of a secondary overdose from the initial ingestion of the opioid, which is why seeking medical attention after an overdose is paramount to survival. Increasing access to naloxone in highly accessible locations—and via mail for more rural locations—can save lives. Naloxone access and basic training on signs of an opioid overdose may increase recognition of opioid misuse and empower the community to provide immediate, lifesaving action.
However, there are concerns that naloxone may end up in a shortage. With its over-the-counter access, naloxone may still be unavailable for those who need it most due to cost (approximately $20 per dose) or access to pharmacies. There is a national push for increasing naloxone distribution, though there are concerns of precursor shortages that will limit or halt production of naloxone. Governmental support of naloxone manufacturing and distribution can assist with meeting demand and ensuring sustainability in the supply chain.
Recommendation 4. Improve training of first responders and medicolegal death investigators.
Most first responders receive training on recognizing signs and symptoms of a potential overdose, and emergency medical and firefighting personnel generally receive additional training for providing medical treatment for those who are under the influence. To avoid exposure to fentanyl, potentially causing a deadly situation for the first responder, additional training is needed about what to do during exposure and how to safely provide naloxone or other medical care. DEA’s safety guide for fentanyl specifically outlines a history of inconsistent and misinformation about fentanyl exposure and treatment. Creating an evidence-based training program that can be distributed virtually and allow first responders to earn continuing education credit can decrease exposure incidents and increase care and responsiveness for those who have overdosed.
While the focus is rightfully placed on first responders as the frontline of the opioid epidemic, medicolegal death investigators also serve a vital function at the intersection of public health and criminal justice. As the professionals who respond to scenes to investigate the circumstances (including cause and manner) surrounding death, medicolegal death investigators must be able to recognize signs of drug toxicity. Training is needed to provide foundational knowledge on deciphering evidence of potential overdose-related deaths, photographing scenes and evidence to share with forensic pathologists, and memorializing the findings to provide an accurate manner of death. Causes of death, as determined by forensic pathologists, need appropriate postmortem examinations and toxicology testing for accuracy, incorporated with standardized wording for death certificates to reflect the drugs contributing to the death. Statistics on drug-related deaths collected by the CDC and public health departments nationwide rely on accurate death certificates to determine trends.
The CDC created the Collaborating Office for Medical Examiners and Coroners (COMEC) in 2022 to provide public health support for medicolegal death investigation professionals. COMEC coordinates health surveillance efforts in the medicolegal community and champions quality investigations and accurate certification of death. The CDC offers free virtual, asynchronous training for investigating and certifying drug toxicity deaths, though the program is not well known or advertised, and there is no ability to ask questions of professionals to aid in understanding the content. Funding is needed to provide no-cost, live instruction, preferably in person, to medicolegal offices, as well as continuing education hours and thorough training on investigating potential drug toxicity-related deaths and accurately certifying death certificates.
Cumulatively, the roughly 2,000 medicolegal death investigation agencies nationwide investigated more than 600,000 deaths in 2018, running on an average budget of $470,000 per agency. Of these agencies, less than 45% had a computerized case management system, which can significantly delay data sharing with public health and allied agencies and reduce reporting accuracy, and only 75% had access to the internet outside of their personally owned devices. Funding is needed to modernize and extend the infrastructure for medicolegal agencies to allow basic functions such as computerized case management systems and internet access, similar to grant funding from the National Network of Public Health Institutes.
Recommendation 5. Fund rapid and thorough toxicology testing in emergency departments and coroner/medical examiner agencies.
Rapid, accurate toxicology testing in an emergency department setting can be the difference between life and death treatment for a patient. Urine toxicology testing is fast, economical, and can be done at the bedside, though it cannot quantify the amount of drug and is not inclusive for emerging drugs. Funding for enhanced accurate toxicology testing in hospitals with emergency departments, including for novel psychoactive substances and opioid analogs, is necessary to provide critical information to attending physicians in a timely manner to allow reversal agents or other vital medical care to be performed.
With the limited resources medicolegal death investigation agencies have nationally and the average cost of $3000 per autopsy performed, administrators need to triage which deaths receive toxicology testing and how in-depth the testing will be. Advanced panels, including ever-changing novel psychoactive substances, are costly and can result in inaccurate cause of death reporting if not performed routinely. Funding should be provided to medicolegal death investigating agencies to subsidize toxicology testing costs to provide the most accurate drugs involved in the death. Accurate cause of death reporting will allow for timely public health surveillance to determine trends and surges of specific drugs. Precise cause of death information and detailed death investigations can significantly contribute to regional multidisciplinary overdose fatality review task forces that can identify potential intervention points to strengthen services and create evidence to build future life-saving action plans.
Recommendation 6. Enhance prevention and enforcement efforts.
DOJ should fund municipal and state law enforcement grants to use evidence-based practices to prevent and enforce drug-related crimes. Grant applications should include a review of the National Institute of Justice’s CrimeSolutions.gov practices in determining potential effectiveness or using foundational knowledge to build innovative, region-specific efforts. The funding should be through competitive grants, requiring an analysis of local trends and efforts and a detailed evaluation and research dissemination plan. Competitive grant funding should also be available for community groups and programs focusing on prevention and access to naloxone.
An often overlooked area of prevention is for justice-involved individuals who enter jail or prison with substance use disorders. Approximately 65% of prisoners in the United States have a substance abuse order, and an additional 20% of prisoners were under the influence of drugs or alcohol when they committed their crime. About 15% of the incarcerated population was formally diagnosed with an opioid use disorder. Medications are available to assist with opioid use disorder treatments that can reduce relapses and post-incarceration toxicity-related deaths, though less than 15% of correctional systems offer medication-assisted opioid use treatments. Extensive case management coupled with trained professionals to prescribe medication-assisted treatment can help reduce opioid-related relapses and overdoses when justice-involved individuals are released to their communities, with the potential to reduce recidivism if treatment is maintained.
DEA should lead local and state law enforcement training on recognizing drug trends, creating regional taskforces for data-sharing and enforcement focus, and organizing drug takeback days. Removing unused prescription medications from homes can reduce overdoses and remove access to unauthorized users, including children and adolescents. Funding to increase collection sites, assist in the expensive process of properly destroying drugs, and advertising takeback days and locations can reduce the amount of available prescription medications that can result in an overdose.
DHS, TREAS, and DOS should expand their current efforts in international trafficking investigations, create additional sanctions against businesses and individuals illegally selling precursor chemicals, and collaborate with countries to universally reduce drug production.
Budget Proposal
A budget of $800 million is proposed to evaluate the current efficacy of drug prevention and enforcement efforts, fund prevention and enforcement efforts, improve training for first responders and medicolegal death investigators, increase rapid and accurate toxicology testing in emergency and medicolegal settings, and enhance collaboration between law enforcement agencies. The foundational research on the efficacy of current enforcement, preventative efforts, and surveillance should receive $25 million, with findings transparently available and shared with practitioners, lawmakers, and community members to hone current practices.
DOJ should receive $375 million to fund grants; collaborative enforcement efforts between local, state, and federal agencies; preventative strategies and programs; training for first responders; and safe drug disposal programs.
CDC should receive $250 million to fund the training of medicolegal death investigators to recognize and appropriately document potential drug toxicity-related deaths, modernize data and reporting systems to assist with accurate surveillance, and provide improved toxicology testing options to emergency departments and medicolegal offices to assist with appropriate diagnoses. Funding should also be used to enhance current data collection efforts with the Overdose to Action program34 by encouraging timely submissions, simplifying the submission process, and helping create or support overdose fatality review teams to determine potential intervention points.
ED should receive $75 million to develop curricula for K-12 and colleges to raise awareness of the dangers of opioids and prevent usage. The curriculum should be made publicly available for access by parents, community groups, and other organizations to increase its usage and reach as many people as possible.
BOP should receive $25 million to provide opioid use disorder medication-assisted treatments by trained clinicians and extensive case management to assist in reducing post-incarceration relapse and drug toxicity-related deaths. The policies, procedures, and steps to create medication-assisted programming should be shared with state corrections departments and county jails to build into their programming to expand use in carceral settings and assist in reducing drug toxicity-related deaths at all incarceration levels.
DOS, DHS, and TREAS should jointly receive $50 million to strengthen their current international investigations and collaborations to stop drug trafficking, the manufacture and sales of precursors, and combating organized crime’s association with the illegal drug markets.
Conclusion
Opioid-related overdoses and deaths continue to needlessly and negatively affect society, with parents burying children, sometimes infants, in an unnatural order. With the low cost of fentanyl production and the high return on investment, fentanyl is commonly added to illicit drugs and counterfeit, real-looking prescription pills. Opioid addiction and fatal overdoses affect all genders, races, ethnicities, and socioeconomic statuses, with no end to this deadly path in sight. Combining public health surveillance with enforcement actions, preventative education, and innovative programming is the most promising framework for saving lives nationally.
Opioid overdoses are occurring all over the nation, including rural areas and tribal communities. Some states have dashboards showing opioid-related deaths by county, similar to the Missouri Department of Health and Senior Services, as do some local county-level health departments like the Washtenaw County, MI Health Department. Mapping programs, such as ODMAP, are available to public safety and public health agencies to watch near-real-time overdose reports, and community organizations may also be tracking overdoses with publicly available information. The CDC’s Overdose Data to Action Program provides data from 47 states and the District of Columbia, producing a robust dashboard separated by participating states and including information about circumstances surrounding deaths and opportunities for intervention.
Community groups can work to spread awareness of opioid dangers and provide preventative education. The DEA has social media resources and a partner toolbox to increase awareness about counterfeit prescription drugs. The National Harm Reduction Coalition has fact sheets and a resource library with webinars and training guides to assist with awareness and prevention campaigns. Community members can also advocate for awareness and preventive education to be added to local K-12 and college curricula. Other key actions are outreach to at-risk populations and empowering parents and guardians to discuss the dangers of opioids with their children.
In 2019, there were approximately 600,000 deaths worldwide related to drug toxicity, with about 80% involving opioids. The United States had 70,630 drug toxicity-related deaths in 2019, 70.6% of which involved opioids, making the country responsible for about 12% of drug-related deaths worldwide. Overdose rates in the United States are significantly overrepresented in drug-related deaths compared to the international population, though data collection and reporting in other countries may not be as robust.
Prior funding to address the opioid epidemic has shown researchers and practitioners what has and has not worked. Despite extensive funding, enacting the National Guard, and creating task forces to combat fentanyl opioid-related overdoses, San Francisco reported 692 drug toxicity-related deaths from January to October 2023, surpassing the 649 deaths in 2022 and the 642 deaths in 2021. San Francisco is on track to have nearly 70 deaths per month, with the final total likely increasing to over 800 by the end of 2023. While this is only one example, the CDC shows an upward predicted value of drug toxicity-related deaths throughout 2023 using national data.
The current funding requests and structure will help to bring forward the dark figures of the epidemic and build robust surveillance systems to track opioid-related toxicities in real time. There are tools available from the pandemic and past opioid use reduction efforts that can be tailored to data collection for opioid-related morbidity and mortality, which, combined with other strategies, can end the opioid epidemic. The increase in overdose awareness and education may be the key to a reduction in overdoses and deaths, similar to how education assisted in curbing human immunodeficiency virus (HIV) transmission. Viewing the epidemic through a public health lens and coupling a pulling-levers approach to crime prevention with educational and data components has the potential to save a significant number of lives.
Troubleshooting Gun Crimes: Prevention To Reduce Firearm-Related Violence
Firearm-related violence is tearing apart the social fabric in the United States. Communities continue to be negatively impacted by the increasing rates of firearm violence, with guns being the leading cause of death for children and young adults (1-19 years of age). Gun-related violence killed over 48,000 people in 2022, a 21% increase from 2019. With more than 130 people dying from firearm-related injuries every day, the Centers for Disease Control and Prevention (CDC) have deemed firearm violence a serious public health issue. While it is challenging to place a dollar amount on the loss of life, injuries, and immediate costs of violence, gun-related violence costs an estimated $557 billion annually, double the U.S. Department of Education Budget for FY 23-24. With the dual epidemic of gun violence and the opioid crisis, coupled with decreased staffing since the COVID-19 pandemic, law enforcement agencies are rapidly running out of resources to battle gun violence to reduce deaths, injuries, and other victimization. A multifaceted approach to preventing gun violence must unite law enforcement, public health, forensic science, community organizations, and education to save lives and reduce continued violence-related trauma.
The Biden-Harris Administration should fund actionable, evidence-based programs for law enforcement, crime laboratories, community organizations, disaster response, and robust data surveillance systems. The Department of Justice (DOJ) would be ideal to provide resources from a law enforcement and forensic science perspective, aided by the CDC, the Department of Commerce (DOC), and the Federal Emergency Management Agency (FEMA) to assist with data collection and analysis, developing standards, and supporting communities impacted by violence. Key recommendations for the prevention of firearm-related violence include:
- Fund law enforcement, crime laboratories, community organizations, and data surveillance.
- Create firearm-related gun violence hubs to support law enforcement efforts.
- Preventative education for youth and adults.
- Provide support to communities recovering from gun violence.
Challenge and Opportunity
Firearm violence continues to significantly affect our communities. Every 11 minutes, someone dies from firearm-related injuries. Underrepresented minority men, especially teens and young adults, account for most firearm deaths. From 2000 to 2020, African Americans were nearly 12 times more likely to be killed in a firearm-related homicide than white Americans. The racial and gender inequities of firearm violence bleed into the community, where disadvantaged and at-risk youth are exposed to high violent crime rates through direct and indirect exposure. Firearm-related violence is associated with many factors, including concentrated disadvantage from areas with high median incomes and significant levels of poverty, racial segregation, poor current and historical police-community relationships, and institutional racism. The media also perpetuates stereotypes of young African American males as assailants but less commonly as victims, putting less importance on the lives of African Americans in the news cycle. Determining the many factors causing gun violence can help prevent further injuries, improve community safety, and transition at-risk youth to at-promise.
In the first eleven months of 2023, there were 619 mass shootings with four or more people shot in the United States, nearly double the number of mass shootings in all of 2017. These mass shootings include school shootings, with 46 shootings in 2022 and 27 in the first nine months of 2023. The shootings resulted in four deaths and 18 injuries, with over 25,600 students on the school campus when the shootings occurred. These do not include shootings on college or university campuses, including two in 2023 at Michigan State University, the University of North Carolina Chapel Hill, and Morgan State University, which resulted in four deaths and 10 injuries. The Morgan State University shooting suspect had a previous felony gun charge that was transitioned to a misdemeanor during a plea bargain, allowing him to purchase guns after his conviction.
The newly established White House Office of Gun Violence Prevention (OGVP) will be monitored by Vice President Harris and aligned with the March 2023 Executive Order to increase firearm purchase background checks and increase red flag laws to remove firearms from perceived dangerous persons. Executive Order 14092 also focuses on firearms reported lost or stolen during the transportation of weapons from the manufacturer to federally licensed firearm dealers, with over 6000 guns lost or stolen during the shipping process in 2022 alone. A renewed focus on the Bipartisan Safer Communities Act of 2022 requires the Secretaries of Health and Human Services, Homeland Security, and Education to provide reports to the President about actions taken to implement the Act and how public awareness and resources were made available to maximize the effects of the Act. Particular attention should be placed on privately made firearms (PMFs), also known as ghost guns, which saw a 1,038% rise in recoveries from 2017 to 2021 and can be easily obtained and constructed without restriction or tracking in most states. Only 13 states have laws restricting PMFs, with the restrictions ranging from requiring serial numbers to background checks for component purchases and not allowing 3D print instructions to be shared (Figure 1). With firearms being deeply rooted in American culture, including being memorialized in the Second Amendment of the Constitution, legal challenges will continue as gun technology changes, new equipment develops to enhance current weapons, and weaponry continues to be available through illicit means, curtailing laws and restrictions.
While laws provide a basis for criminality, law enforcement action is needed to recognize and investigate gun-related crimes, and district attorneys must commit to prosecuting crimes. Significant staffing issues continue to plague law enforcement, limiting the ability to reduce violent crime, act proactively, and work with the community to build healthy relationships. Forensic evidence collection and processing are vital to investigation and prosecution, requiring personnel, training, standards, and technology that is not universally accessible to criminal justice agencies. Law enforcement participation in task forces and collaboration with federal, state, and local partners, including prosecutors, can reduce gun violence but requires significant resources and personnel that are not currently available in all jurisdictions. Law enforcement agencies publicly stating they will not enforce gun laws and emergency orders work against the necessary joint vision and actions needed to reduce violence.
Examining the efficacy of past firearm-related crime interventions and community efforts while seeking innovative solutions can help build robust and successful gun violence prevention efforts across the nation. No single program or intervention will work for all jurisdictions, so data-driven implementation and research efforts will be required for each community to adequately combat firearm-related crime. Community-based intervention programs vary from local nonprofit organizations and religious groups to national think tanks working with the common goal of reducing violence and improving community well-being. As the causes of gun violence vary by community and region, having non-law-enforcement entities and social workers employed in collaboration with criminal justice agencies may improve well-being and safety while reducing violence. Treating gun violence as a public health issue is an important allied approach to enforcement since public health focuses on research-based avenues to reduce morbidity and mortality. A public health lens can assist in examining societal structural and social factors while reducing the political aspect that can affect gun violence tactics. Public-health-related gun violence research was severely limited by the Dickey Amendment in 1996, which restricted federal funds to advance gun control or gun violence research. With the 2018 omnibus spending bill passed to support firearm-related research, there has not been a significant change to funding, continuing to limit funding for the CDC to research the causes of gun violence.
Plan of Action
Addressing the many aspects of gun violence, including preventative education, requires a multifaceted approach. Collaboration between federal, state, and local government agencies and community organizations is necessary to determine and address gun violence and preventative efforts. The additional details of federal agency involvement and their governmental roles are below.
Recommendation 1. Fund law enforcement, crime laboratories, community organizations, and data surveillance.
The DOJ should fund action-oriented efforts for states and local law enforcement agencies to focus on reducing firearm-related violence. Creating regional task forces can assist in data-sharing and firearm-specific crime reduction tactics with additional resources and personnel. Funding should also be available to update report management systems to assist with evidence tracking, trends to modified weapons, and types of magazines used, especially the involvement of extended magazines.
Funding of accredited crime laboratories can help expand the use of the National Integrated Ballistics Information Network (NIBIN), which allows cartridge cases found at crime scenes to be matched to guns and other crimes. Training additional ballistics specialists and increasing NIBIN submissions can link more crimes and increase enforcement efforts. NIST should develop and broadcast standards for ballistic evidence collection and processing to assist law enforcement and forensic scientists in improving evidence recovery and analysis as technology and techniques improve. With firearm evidence backlogs persisting, funds for personnel, equipment, and processing costs to assist with the timely submission of firearm-related crime evidence are necessary to improve evidence collection and processing efforts.
The DOJ should also fund community violence intervention programs spearheaded by local nonprofit and street outreach organizations. With continued distrust of police, especially in the most violent of areas, community-based intervention programs can focus on crime prevention through environmental design, working with at-risk/at-promise youth, and mediating conflicts that do not escalate to require law enforcement intervention.
All DOJ funding should require successful evidence-based practices, such as those outlined in the National Institute of Justice’s CrimeSolutions.gov, and data collection and evaluation to determine effectiveness. Funding should be competitive grants, studying trends, root causes, and community efforts to reduce gun violence. Researchers should convene at a national firearm-related crime prevention symposium to discuss findings, determine regional and national trends, and outline recommendations to prevent firearm violence.
The CDC should fund real-time data collection efforts to support the National Crime Victimization Survey by hiring more epidemiologists and data entry specialists, expanding current research efforts on firearm violence and injury prevention, and public health-related grants focused on reducing firearm morbidity and mortality. Research and reports, especially resources for action, should be expanded to include firearm-related injuries and deaths and assist with providing comprehensive planning and policy work to communities to combat gun violence. Data modernization efforts are needed to encourage auto-reporting of gun-related incidents from law enforcement, emergency medical services, and hospitals to increase accuracy and real-time reporting and surveillance.
Recommendation 2. Create firearms-related gun violence hubs to support law enforcement efforts.
Gun violence hubs are regional resources involving multiple levels of criminal justice agencies to share data, assets, and strategies. A hub in central Ohio involves local and state law enforcement, a narcotics intelligence center, Attorney General investigators, and the ATF, which has been vital to linking crimes and aiding in gun crime prosecution. While some large law enforcement agencies, such as Los Angeles and New York City Police Departments, have the resources to run gun crime-related intelligence centers with in-house investigative and forensic personnel with modern technology, most agencies do not have similar capital. Federally funded state-wide or regional hubs in larger states can provide the necessary personnel, funding, and intelligence to battle gun violence while incorporating community intervention programs to ensure alignment with efforts. Vigorous research on efforts and robust data sets are needed to accurately guide future interventions and actions, instead of anecdotal evidence relating to policy implementation that can currently shape programming. The research results should also be made available open-source and presented at local, state, and national levels to share information about implementation and findings.
Increasing communication and pooling resources can help break down traditional silos in local, state, and federal law enforcement. Incorporating community groups into gun violence prevention efforts can bring information and programming closer to the people who need assistance without directly incorporating law enforcement with community efforts. Community violence intervention programs, targeting the most at-risk of victimization and breaking cycles of retaliatory violence, can work in concert with law enforcement efforts, sharing data and resources. Community programs can also assist in using a public health and racial equity lens to determine the root causes of violence and advocate for victims in underserved communities.
Recommendation 3. Develop preventative education for youth and adults.
The Department of Education should create gun violence prevention education and integrate it into all levels of education. The educational program should focus on gun safety when guns are encountered at home; handling pressure to participate in violent activities, including gang membership; situational awareness and safety in mass shooting situations; and anger management. The educational efforts for students can be extended to adults through social media marketing with television and streaming service advertisements. The DOJ should enhance educational requirements when purchasing weapons and ammunition. The DOJ should also complete widespread information sharing about red flag laws for reporting someone who exhibits risks of violence to help save lives while protecting the rights of the person reported.
Advertising to youth was shown to promote tobacco usage, and marketing was also shown to influence gender and ethnic communities to use tobacco. The CDC can evaluate how gun manufacturers market firearms to minors to determine how the marketing can affect health trajectory.
Recommendation 4. Provide support to help communities recover from gun violence.
Over 4,500 children and teenagers were killed by gunfire in 2022, making gun violence the leading cause of death for this age group. From 2013 to 2022, there was an 87% increase in gun deaths of children and teenagers, with Black youth 20 times more likely to be killed by firearm violence than white youth. The racial disparity in firearm-related deaths can be tied to generational inequities in our health, housing, justice, and educational systems coupled with police mistrust and hurdles to access victim services. Community violence, especially when children and teenagers are shot and survive, has a significantly negative impact on mental health and substance abuse. In the year after a child or adolescent suffered a gunshot injury, research found a nearly 120% increase in pain disorders, an almost 70% increase in psychiatric disorders, and a nearly 145% increase in substance abuse disorders. Parents of survivors have an approximately 30% increase in psychiatric disorders with a reduction of mother and sibling routine healthcare appointments. The mental health and disorder effects on children and adolescents were similar to adult gun violence survivors, who also had significantly increased healthcare costs post-injury. Gun violence effects ripple far from the victims and families and also affect community mental health and healthcare costs.
FEMA offers financial, medical, and mental health resources during and after disasters while working to improve preparedness, response, and recovery efforts from hazards. Traditionally, FEMA response has been to declare disasters, primarily natural disasters, governed by legal authorities of disaster response. New Mexico Governor Michelle Lujan Grisham declared a public health emergency in September 2023 relating to gun violence, though the emergency did not enact a federal response or recovery from FEMA. New York Governor Andrew Cuomo formally declared a disaster due to gun violence in July 2021 via executive order, which was extended in April 2023. FEMA helped ensure Medicare was extended through the disaster time frame, though no other federal resources were provided. Amendments to disaster acts should include mass shootings with eight or more injuries/deaths, which would be considered mass casualty incidents in many jurisdictions. Funding through FEMA can provide medical and other basic needs resources, enhance safety efforts, strengthen social infrastructure, and promote resilience. FEMA has funded similar programs around building resilient infrastructure relating to hazard mitigation with disasters and natural hazards, promoting partnerships, and building capacity for innovation. FEMA’s Office of Emerging Threats could be used to handle gun violence disaster requests, make connections between data and risk, and bring another layer of operational planning and response to communities from a recovery aspect. FEMA’s Preparedness grants can also be extended to include gun violence, another funding opportunity for local governments and communities.
Budget Proposal
A budget of $500 million over five years is proposed to evaluate the efficacy of current interventions; fund criminal justice, public health, and community intervention organizations; and create preventative gun violence-related education. The foundational research on the current interventions should receive $20 million, requiring transparent findings and a research conference available to practitioners, lawmakers, and community members to share data and assist with determining future research and grant-funding directions.
DOJ should receive $320 million to fund grants, collaborative efforts, community violence intervention programs, gun violence hubs, enhancement of evidence recovery and processing, and development of criminal justice-related standards to improve investigations and prosecution rates. Competitive grants should be offered in addition to guaranteed funding for states willing to create regional task forces and gun violence hubs. All funding should require an evaluation component with results available publicly without paywalls on the Office of Gun Violence Prevention website.
ED should receive $50 million to develop curricula to prevent gun violence and fully integrate it into the grade-specific curriculum for K-12 and require education in colleges. The educational materials created, especially at the college level, will be made public for use in community training programs, ads to reduce gun violence, and other applicable settings.
FEMA should receive $100 million to respond to communities affected by gun violence to provide a disaster response. The Federal Trade Commission should receive $5 million to investigate the marketing of firearms to youth and military-style weaponry. An evaluation of the entire proposal should be funded for $5 million after five to eight years of expected evaluative work. The final report will be made public, in addition to annual progress reports, and available transparently on government websites.
Conclusion
Gun violence negatively affects the lives of Americans daily, with no end in sight. Firearm intervention efforts and enforcement tend to lack collaboration, data-driven insights, focus on root causes, and sustainable funding. The widespread exposure to gun violence and societal inequities in communities are generally not addressed, though they can lead to significant health and well-being impacts and a continued cycle of violence. Reducing gun violence requires a comprehensive approach through a public health lens involving community input and intervention while creating awareness of effective legal and policy strategies.
A shared framework between all federal, state, and local agencies is necessary to align priorities, resources, and efforts to mobilize evidence-based initiatives, collect data, and prevent gun violence. Congregating researchers, practitioners, community members, and lawmakers at a firearm-related violence symposium to share efforts, research findings, and outline future paths will be vital to violence prevention nationally. Mobilizing disaster-response-level support to communities affected by gun violence and providing preventative education can provide resources to heal and help break the cycle of violence while providing opportunities for social mobility.
The youth firearm-related death rate is ten times higher in the United States than in the next country of similar wealth and size. In 2021, 6 per 100,000 U.S. youth aged 1-19 died due to firearms. Canada had firearm mortality rates of 0.6 per 100,000 people, followed by Austria, France, and Switzerland with 0.3 per 100,000 deaths. Motor vehicle and pedestrian deaths are the top cause of death in youth in Australia, Austria, and Canada, with cancer being the leading cause of death in Germany, Japan, and the Netherlands. Expanding to all age ranges in the United States, Mississippi had 33.9 firearm-related deaths per 100,000 people, followed by Louisiana with 29.1.
President Biden’s March 2023 Executive Order addressed the need for universal background checks nationwide and increased red flag laws, furthering the Bipartisan Safer Communities Act from 2022. The Safer Communities Act included legislative changes to enhance background checks, including into juvenile mental health records, and provide funding to drug courts and intervention programs. The Office of Gun Violence Prevention will have the monumental task of implementing legislative policy, determining the efficacy of current efforts, and investigating leverage points that can assist in reducing and ultimately preventing gun violence.
About half of gun violence can be associated with 5% of city blocks, which are generally underrepresented minority-inhabited neighborhoods. A FEMA-style disaster response to these areas can provide a health and structural foundation to the community, while community-based intervention programs can provide economic and opportunity efforts to help reduce violence. Research on root causes of violence in regions and communities can hone in on areas-specific concerns while determining inequalities that can fuel gun violence.
Community violence intervention programs are local organizations focused on reducing violence in their communities through innovative, non-enforcement-based efforts. Examples of community violence intervention programs include the Alliance for Concerned Men in Washington, DC, the Institute for Nonviolence Chicago in Chicago, IL, No More Red Dots in Louisville, KY, and YouthAlive! In Oakland, CA.
The City of Oakland offered micro-grants to community organizations to promote community healing and gun violence reduction. The grassroots community efforts fund community members and small nonprofits to enact change from the epicenter of violence, which tends to be more well-received than outside efforts to support communities.
The National Institute of Justice’s CrimeSolutions.gov rates research programs on effectiveness and has over 400 research results involving community violence and intervention programs. A review of rated programs can help determine which efforts can work in different regions, and following evidence-based research can lead to programmatic success.
The economic impact of gun violence is over $550 billion annually in the U.S. Gun violence research was officially funded by the federal government for the first time in 2020, allocating $25 million to the CDC and National Institutes of Health. At a state and local level, hundreds of millions of dollars are spent on grant funding through federal, state, and philanthropic funding arms, though research findings regularly end up behind academic journal paywalls and are inaccessible to law enforcement and community members. Continuing to fund firearm-reduction efforts will allow the successes of current programs to be appropriately evaluated and data to be shared with researchers and practitioners. Withdrawing funding may take programming and resources from the most vulnerable members of our community, potentially increasing injuries and deaths.
This funding request focuses on reviewing past efforts to determine program efficacy, incorporated with increasing collaboration and resources beyond jurisdictional lines, gun violence prevention education at all grade levels, and a focus on providing financial and health-related resources to communities affected by gun violence to break the cycle of victimization. The combined efforts bring an interdisciplinary approach to an increasingly complex problem that is costing over 100 lives daily.
Improving Public Health by Advancing the Medicolegal Death Investigation Profession
Medicolegal death investigations produce vital information on fatal illnesses and injuries in the United States, yet the system is fractured and underfunded. Less than half of deaths are reported and investigated by medicolegal death investigation agencies. In addition to providing cause and manner of death determinations, the investigations are instrumental in identifying public health trends, including early identification of the opioid epidemic and fatal fentanyl overdoses. Data from death investigations is used by over 40 federal agency programs in creating policies and regulations. Medicolegal death investigations agencies are generally underresourced, with insufficient infrastructure for data-sharing and computerized record management. These critical shortfalls are combined with a dire shortage of board-certified forensic pathologists to complete postmortem examinations and a lack of mass fatality preparedness, which can directly affect community health and well-being.
The last time medicolegal death investigation policies were reviewed by the Executive Branch was during the Obama Administration. In 2016, the National Science and Technology Council (NSTC) Committee on Science’s Medicolegal Death Investigation Working Group noted the essential role medicolegal death investigation agencies play in establishing a scientific cause and manner of death while serving public health and reporting emerging health threats. The working group outlined the importance of accrediting medicolegal death investigation offices and certifying medicolegal death investigators. In the seven years since the report, there has only been an increase of 23.7% in certified death investigators, with more jurisdictions requiring certification to maintain employment. The NSTC’s Fast-Track Action Committee found the need to improve infrastructure and support for medicolegal death investigation agencies to reinforce the integrity of public health and criminal justice systems.
Key recommendations for improving public health by advancing the medicolegal profession include:
- Creating national foundational medicolegal death investigation training standards.
- Funding data infrastructure modernization and enhanced surveillance efforts.
- Researching the current efficacy of mass fatality response policies and efforts to create standardized procedures.
- Increasing certification and accreditation to enhance professionalism, knowledge, and skills.
- Supporting forensic pathologist pathways and debt reduction.
Challenge and Opportunity
Medicolegal death investigation is at the intersection of medicine, public health, and the criminal justice system, yet it does not have a formal place in any system nationally. Public health trends, including early detection of outbreaks and emerging health threats, are found during autopsies and reported on death certificates. The data from death certificates is used in public health surveillance at a local, regional, state, and national level to determine trends and the impact of interventions, shape policy, and help recognize health disparities. The information from the death certificates is obtained through death scene investigations, evidence collection, medical record reviews, postmortem examinations, and toxicology testing, coupled with interviews of witnesses, family, and friends of the decedent. Data obtained during medicolegal death investigations not only provides an accurate cause and manner of death but also helps the living by showing the health of our communities and tracking death trends and health threats.
The coroner system in the United States stems from the English system dating to the 12th century. A physician-headed medical examiner system was created in Massachusetts in the late 1800s, leading to versions of our current systems. State statutes and local jurisdictional charters create the structure of medicolegal death investigation offices. There is no standardized medicolegal death investigation system across the United States. Coroners are typically elected officials who run for the political role through normal voting processes. Coroners can also be appointed based on the jurisdiction and are regularly non-medical professionals. In contrast, medical examiner’s offices generally have a physician leading the office, except in Wisconsin, where the appointed medical examiner can be a non-physician. The jurisdiction of a coroner or medical examiner’s office is most commonly a county, though 16 states have a centralized state medical examiner system. There are 14 states with a county or district-based coroner system, 14 states with a mixture of coroner and medical examiner offices, and six states with county or district medical examiner systems. Texas has Justice of the Peace positions where the elected role hears misdemeanor, traffic, and civil disputes in addition to holding medicolegal duties without a requirement for any legal or medical experience or education. California is unique with four different medicolegal investigation agency types, including a Sheriff-Coroner, Coroner, Medical Examiner, and Coroner-Medical Examiner. The Sheriff-Coroner’s position, which is in 48 of California’s 58 counties, is the most contentious due to concerns about the independence of investigations when the medicolegal agency head also serves as the sheriff. A 2022 attempt to separate sheriff and coroner positions was unsuccessful. Medicolegal death investigation agencies range from having one part-time elected official responsible for the entire jurisdiction to having over 100 employees, with most agencies across the nation having few full-time employees and significantly limited resources.
The varied names and jurisdictions for medicolegal death investigation offices do not change the foundation of the duties: investigating unexpected and unnatural deaths. Typically, the medicolegal death investigation agency receives a call from a law enforcement agency, medical first responder, hospital, care facility, or other medical professional to report a death. Basic demographic information, the known circumstances behind the death, medical history, and other vital information are obtained to determine jurisdiction. Based on agency practices and state law, the medicolegal death investigator may respond to the death scene to assume jurisdiction and custody of the decedent. For natural deaths where a physician will certify the death to natural causes, the medicolegal death investigator may be able to release the decedent to a funeral home or mortuary of the family’s choice. When a medicolegal death scene investigation is required, the investigation includes photography, collecting evidence, identifying the decedent, locating and notifying kin, writing an investigative report, and providing information to the forensic pathologist, who will determine the cause of death. Death certificates are commonly generated by the medicolegal office, with the manner of death determined by the chief medicolegal officer. Medicolegal death investigation offices are also tasked with identifying decedents, which may require advanced scientific testing. Less than 50% of medicolegal agencies collect DNA samples from unidentified decedents, which is essential in present-day scientific identification and adds information to national databases. Not collecting DNA can significantly delay the identification of decedents and notification to friends and family of missing and unidentified people.
Medicolegal death investigation offices also participate in specialized fatality review teams, which include multidisciplinary stakeholders from social services, public health, law enforcement, emergency medical services, and other areas to find systemic gaps in treatment and identify potential missed intervention points. Fatality review teams can be regional and can include overdose fatality review, infant and child death fatality review, domestic violence fatality review, and elder abuse fatality review. Meeting findings are summarized into actionable items to prevent future deaths. The medicolegal investigative and autopsy reports and the reviewed medical and social history provide the requisite information to allow the multidisciplinary teams to make prevention determinations.
Medicolegal death investigation agencies report to local, state, and national organizations to assist with surveillance and injury prevention. Many states require medicolegal death investigators to report workplace injuries and deaths to the regional Occupational Safety and Health Administration branch, with death certificates reporting contagious diseases and drug toxicity-related deaths to local health departments. The United States Consumer Product Safety Commission relies on medical examiners and coroners to report consumer product-related deaths so they can further investigate products, create appropriate warning labels, and potentially prevent injuries and deaths. For deaths relating to medical misadventure, medicolegal death investigation agencies must also report deaths to the state medical board, dental board, nursing board, or county-level emergency medical services board. There are two national reporting systems, both overseen by the Centers for Disease Control and Prevention (CDC), for violent deaths and overdoses. The National Violent Death Reporting System records violent death data from medicolegal and law enforcement reports to link over 600 data points to create a context behind the death and develop violence prevention strategies. The State Unintentional Drug Overdose Reporting System oversees 49 states and Washington, DC, to obtain inclusive overdose fatality data. The data includes information on the known circumstances behind the death and identification of the substances involved to gain nearly real-time information about emerging drug threats and determine the effect of prevention efforts. Coroner and medical examiner agencies may also be required to enter unidentified persons into missing and unidentified person systems and the National Missing and Unidentified Persons System to assist with future identification efforts. Data review and entry are complicated, with limited resources, a lack of case management systems, and time constraints with part-time employee offices.
The data and information obtained from medicolegal death investigations have many uses that can assist in local, state, and national prevention efforts. The challenges for the reporting systems are that they are voluntary, and many agencies do not have the resources to provide hundreds of data sources to multiple systems. Having data organized and in a searchable database is key for access and data-sharing, though less than 50% of medicolegal offices with a population of less than 250,000 people have a computerized case management system. Only 87% of agencies with a population of over 250,000 people have a case management system, with 40% of coroner offices not having internet access outside of their personal devices. Computerized case management systems help reduce errors and lost paperwork while increasing efficiency and resource allocation. Less than 70% of coroner offices have access to fingerprint databases, compared to 91% of medical examiner agencies, and 82% of agencies have access to bloodborne pathogen training. The average budget of a medicolegal office is $470,000, with each decedent autopsy and investigation costing approximately $3000. With about 2,040 medicolegal death investigation offices nationally and almost 11,000 full-time equivalent employees, there is an average of just five full-time employees per office. A large portion of the budget is commonly spent on personnel, leaving little funding for improving infrastructure and training.
There is no standardized oversight or required training of medicolegal death investigation personnel. Only 16 states require training for medicolegal death investigations. For example, California requires 80 hours of training for medicolegal death investigators, the highest of all state requirements. In contrast, New York requires training for the coroner and deputy coroners but does not outline the required number of hours or duration. The American Board of Medicolegal Death Investigators (ABMDI) is a national certifying board that the Forensic Specialties Accreditation Board accredits. ABMDI tests medicolegal death investigators on foundational and advanced knowledge, awarding registry and board certifications. ABMDI certification requires continuing education to maintain certification, though most medicolegal agencies do not require certification for employment. The lack of standardized training of medicolegal death investigation personnel can lead to gaps in knowledge and recognizing evidence, dramatically reducing the accuracy of death certificates and reporting. Limited budgets, personnel, and resources contribute to a lack of investigative awareness that can lead to incorrect causes and manners of death. Inaccuracies on death certificates can have a profoundly negative effect on families and the community and contribute to public mistrust.
Training is not the only constraint in accurate and timely medicolegal death investigations. There is an extreme shortage of board-certified forensic pathologists, who are the physicians conducting postmortem examinations and determining the cause of death. In 2020, there were approximately 500 practicing forensic pathologists, but the workload required 1,280 forensic pathologists. The gap is now likely even greater, with workloads having increased with the rise of the opioid epidemic, fentanyl deaths, gun violence, and COVID-19. The 2018 coroner/medical examiner census noted 890 forensic pathologists employed by medicolegal agencies, though forensic pathologists commonly work in neighboring counties or other states as a locum tenens, a temporary, per-diem physician. The shared nature of some forensic pathologists inflates the number of physicians who appear to be working, shrouding the significantly lower number of practicing physicians. In medical examiner officers, such as in Los Angeles and New York City, the department head is a forensic pathologist assigned solely to administrative work, limiting the number of available forensic pathologists to complete postmortem examinations. Some jurisdictions resort to using non-board-certified forensic pathologists for postmortem examinations, which can result in inaccurate causes and manners of death. The lack of available forensic pathologists also allows for non-qualified people to falsify credentials and autopsy reports, even in high-profile cases, defrauding grieving people and the government alike. A 2015 report on increasing the number of board-certified forensic pathologists mentioned that physicians should work in a nationally accredited office. Agency accreditation is important to ensure proper working conditions and a high standard for policies and procedures to create an environment for the best possible medicolegal death investigations. Yet the last coroner/medical examiner census showed that only 17% of medicolegal death investigation offices were accredited. Some agencies will never be able to reach accreditation, as there is a limit of 325 autopsies per year, and workload shortages restrict the number of available forensic pathologists to complete autopsies.
The medicolegal profession is highlighted in the media in high-profile deaths and mass fatality situations. A significant amount of time and effort by medicolegal administrators should be devoted to mass fatality planning to provide an efficient, effective response, coordinate with allied agencies, and safely recover and identify decedents. There is no specific number for what constitutes a mass fatality incident, as mass fatality is when the number of deaths exceeds agency resources. In some jurisdictions, a mass fatality may be three decedents from one incident, while others may request allied resources when 50 decedents are from an incident, such as in the October 1, 2017 mass shooting in Las Vegas, NV. All states have an Office of Emergency Response or similarly named emergency response commission, where medicolegal death investigation agencies should be integrated into mutual aid and planning committees. There are significant limitations with the response to and accurate handling of medicolegal death investigations without a case management system and internet access, impacting smaller and underresourced jurisdictions. The federal-level Disaster Mortuary Operational Response Team (DMORT), run by the National Disaster Medical System, deploys to mass fatality scenes to assist with recovery, examination, identification, and collecting ante- and postmortem decedent data. DMORT responds with qualified personnel, including forensic pathologists and investigators, to set up a mobile autopsy suite and bring decedent storage facilities. With the high cost of deployment, DMORT only responds to large-scale mass fatality scenes and needs to be requested by a state Office of Emergency of Response when other mutual aid responses have been exhausted. A vast majority of medicolegal agencies lack the resources to handle a mass fatality. Less than 30% of agencies had specialized response training, and nearly half of agencies reported that they were only moderately prepared for a mass fatality.
The challenges of advancing mass fatality planning and improving medicolegal infrastructure are restricted by agency budgets and limited grant funding. Due to the specialty of the field and because it crosses the medicine, public health, and the criminal justice systems, there are few federal grant opportunities. The Bureau of Justice Assistance’s Strengthening the Medical Examiner-Coroner System Program helps with accreditation, including purchasing supplies and upgrades to meet standards and assisting with funding for forensic pathology fellowships. There were 14 awards in 2023 totaling over $2 million, with funding ranging from $53,878 to $300,000. Most of the awards were to larger agencies, including Los Angeles and New York City, where there are resources for grant writing and administration. The competitive Paul Coverdell Forensic Science Improvement Grant Program is offered to forensic science and medicolegal agencies with forensic science laboratories. In 2023, more than $4.6 million was awarded to 15 agencies, with only one grant awarded to a medicolegal death investigation agency. The National Network of Public Health Institutes funded $200,000 to 10 medicolegal death investigation agencies in 2023 to improve data collection from medicolegal agencies for surveillance of overdose-related mortality reporting. Nationwide, there are more than 2,000 medicolegal death investigation agencies, but in 2023 just 25 received federal or national-level grant funding.
Plan of Action
A multi-stage, multi-agency approach is needed to improve medicolegal death investigations in the United States to provide accurate mortality data to shape prevention and policy efforts. In addition to increasing minimum medicolegal death investigation operating budgets, funding is needed to improve training, attract physicians to forensic pathology, and advance infrastructure upgrades for timely and accurate mortality data reporting. National standards for medicolegal death investigation should be established and integrated into state systems for reliable, reproducible, and scientifically valid investigative results and analysis.
Recommendation 1. Create national foundational training standards.
Building from the National Institute of Justice’s 2011 Death Investigation: A Guide for the Scene Investigator Technical Update and fundamental tasks of medicolegal death investigation from the American Board of Medicolegal Death Investigators, the NIST should convene a multidisciplinary group of subject matter experts to develop foundational training standards guided by NIST’s Organized Scientific Area Committees for Forensic Science best practices and standards. The DOL should be involved in reviewing and structuring training standards and programming from a labor and workforce perspective. Subject matter experts should determine a continuing education structure to allow for continuous training for contemporary topics in the field, similar to requirements for maintaining medical licensure. Although NIST is not an enforcing agency, the created standards should be made widely available to state legislation and the medicolegal community. States that adopt the standards should have access to additional NIJ funding to improve medicolegal offices. Similar to NIJ funding requiring credentials for discretionary funding for law enforcement agencies for use-of-force policies and the prohibition of chokeholds, the discretionary funding can be limited to agencies that have adopted the NIST standards.
Funding for training should be available through grants and legislation for funding from burial permits. Since 1991, California has designated $1 from each burial permit to fund medicolegal death investigation training. Creating similar legislation for every state can allow for sustainable funding for continued training, alleviating the need for continued federal funding.
Foundational training standards will create a minimum and standardized training nationally to improve medicolegal death investigations and utilize best practices to best serve communities. The training will also allow medicolegal death investigation agencies to provide more accurate and timely data for public health surveillance and participate in multidisciplinary task forces, which can potentially reduce future deaths. Requirements for foundational and continued training can be shared widely by COMEC, with virtual training programs created by COMEC and available for continuing education credit. COMEC currently hosts virtual training for sudden unexpected infant death investigation, the investigation and certification of drug toxicity-related deaths, and death investigation after natural disasters and radiation emergencies. Existing training and structure can be used to create and distribute foundational training and continuing education at a national level without reinventing a new nationally available website and training structure.
Recommendation 2. Fund data infrastructure modernization and enhanced surveillance efforts.
The health of communities lies in early recognition and timely reporting of causes of death. With less than 50% of medicolegal death investigation agencies having a computerized case management system and under 40% of coroner offices having business-related internet access, the field cannot progress without a significant investment in infrastructure. The lack of computerized case management will continue to severely limit timely data-sharing with local, state, and federal public health agencies, restricting near real-time analysis of death trends and disease tracking. Public health surveillance of mortality data assists in recognition, intervention, and preventive efforts, which cannot be accurately completed without timely and complete data from medicolegal death investigation agencies.
With the current state of the opioid epidemic and fentanyl drug toxicity-related deaths, rapid and accurate toxicology testing is needed for public health surveillance. Advanced toxicology panels, including the ever-growing novel psychoactive substances, are expensive, and agencies need to make difficult budgetary decisions around personnel and toxicology testing. Funding is needed to subsidize advanced, rapid toxicology testing to provide the most accurate types of drugs involved with the death. Additional funding, awarded through a cooperative agreement by the CDC, should be allocated to advanced panel toxicology testing and the purchase of rapid toxicology screening machines that can be housed in the medicolegal office. Rapid toxicology screening machines do not quantify all drug levels, which commonly requires secondary toxicology testing through an accredited laboratory. But the screening does allow for nearly immediate identification of fatal drug trends, allowing for early notification to public health officials. The NIJ should specifically request research and development of a rapid toxicology testing process with an accuracy level that does not require secondary testing in their research grant for forensic science for criminal justice purposes to provide additional options for medicolegal agencies. The precise cause of death, involved drugs, and thorough investigations significantly contribute to multidisciplinary overdose fatality review teams. The fatality review teams can use the information to identify timely intervention strategies and strengthen services to reduce future drug toxicity-related deaths in near real-time.
Recommendation 3. Research the current efficacy of mass fatality response policies and efforts to create standardized procedures.
In the focus on current caseload and office needs, mass fatality preparedness and training tend to be overlooked. This deprioritization is dangerous for medicolegal death investigation personnel responding to scenes and is concerning for the community with underprepared and underresourced investigators working to navigate a mass fatality incident. The declaration of a federal state of emergency does not always provide funding for medicolegal death investigation agencies for fatality management operations, and the nature of the mass fatality may limit mutual aid response to assist jurisdictions, such as in the case of earthquakes, biological acts of terrorism, and other large-scale natural disasters. Research is needed to determine best practices in mass fatality planning and resourcing for all jurisdictional sizes, including determining the current state of planning and available resources. DOJ should fund the research through BJA or BJS via a grant process to find the most qualified and knowledgeable researchers. Findings should be shared widely via open-source academic journals, at national and regional medicolegal conferences, and via webinars to ensure the information is readily available. The findings should also be published in a guide on the DOJ website to assist agencies in creating personalized mass fatality plans and practical exercises.
Recommendation 4. Increase certification and accreditation to enhance professionalism, knowledge, and skills.
The National Commission on Forensic Science supported recommendations for the accreditation of medicolegal death investigation offices and the certification of medicolegal death investigators in 2015. Despite these recommendations, only 17% of medicolegal death investigation offices were accredited in 2018. In November 2023, there were 2,049 actively certified diplomates with the American Board of Medicolegal Death Investigators, from an approximate 11,000 full-time equivalent positions, totaling approximately 19% of full-time equivalent medicolegal death investigators. Increasing the number of accredited offices and certified medicolegal death investigators can provide consistency in practice, improve data quality, enhance facilities, incorporate evidence-based best practices, and elevate surveillance efforts.
Recommendation 5. Support forensic pathologist pathways and debt reduction.
There is no end in sight to the critical shortage of forensic pathologists, who are neutral scientists specializing in determining the cause of death while providing valuable data for public health surveillance. A federal grant is available to provide a stipend for forensic pathology fellows in training, including limited loan repayment and travel for fellowship recruitment. Funding is limited and requires medicolegal death investigation agencies to be knowledgeable about the grants and be awarded funding. A more grassroots approach to creating more forensic pathologists should begin earlier, both in medical school and in offering scholarships for current medicolegal investigative personnel to attend medical school to become forensic pathologists. The field should be highlighted during the early years of medical school, requiring a rotation through a local medicolegal death investigation office, and increasing residency and fellowship pay to encourage physicians to enter the field and become board-certified. Similar to other loan repayment programs, loan forgiveness for forensic pathologists should be reduced to five years in public practice as a board-certified forensic pathologist. Funding should be provided to medical schools, residency, and fellowship programs and not dependent on a limited competitive federal grant funding process.
Budget Proposal
A budget of $90 million is proposed to create national medicolegal death investigation training standards, fund data infrastructure modernization and enhance surveillance efforts, research the current efficacy of mass fatality response, increase medicolegal certification and accreditation, and support forensic pathologist career pathways. NIST should receive $2.5 million to hire and support subject matter experts to create the national foundational medicolegal death investigation training standards. The DOL should be awarded $500,000 to support standards development with a focus on the workforce and labor. Circulating the standards through a standards-developing agency, such as the American Academy of Forensic Science’s Academy Standards Board, should occur at no cost.
The CDC should be provided with $32 million to create and manage low-barrier infrastructure improvement grants focusing on smaller and medium medicolegal jurisdictions to ensure agencies have computerized case management systems and basic internet connection at a minimum. Medicolegal death investigation data elements for reporting and information exchange have been outlined by the Medicolegal Death Investigation Subcommittee of NIST’s Organization of Scientific Area Committees, providing a baseline of data needs for a computerized case management system. At least $1 million of the funding should focus on low-barrier scholarship-type funding for individual medicolegal death investigator certification, with the certifying agency accredited by the Forensic Specialties Accreditation Board for monitoring professional board certification. At least $5 million should be available for low-barrier grants to assist medicolegal agencies in achieving accreditation through one of the two medicolegal death investigation agency accreditation boards. Annual reporting on the number of agencies and individuals funded for infrastructure improvements, accreditation, and certification should be transparently listed on the CDC funding website.
The DOJ should receive $4 million for nationwide research on the efficacy of mass fatality response policies and the creation of standardized procedures. Portions of the funding should be dedicated to open-source publishing to allow broad access to the research findings, with a guide on best practices and standards made available on a federal government website to help agencies create and hone their policies. The information should also be presented at national, state, and regional medicolegal and forensic science conferences with at least one recorded webinar to provide data and support to the most agencies possible.
Similar to providing grants for physicians and healthcare professionals to work in health professional shortage areas, medically underserved areas, or primary care shortage areas, funding should be provided to state Departments of Health Care Access and Information or similarly positioned state-level departments. Each state and the District of Columbia should receive $1 million for scholarships, loan forgiveness, and fellowship reimbursement for physicians on track to become board-certified forensic pathologists. State funding should also be used to introduce forensic pathology as a subspecialty during medical school rotations to provide exposure to the career.
Conclusion
The current state of medicolegal death investigations in the United States is plagued with significant variations in practices, budgets, and training across jurisdictions. The heterogeneity creates disparities in the quality of investigations, data reporting, participation in fatality review teams, and overall professionalism in the field. The continued shortage of board-certified forensic pathologists to complete postmortem examinations and the lack of standardized training exacerbates the challenges. Increased federal funding to support medicolegal death investigation efforts can lead to more accurate and timely data reporting, improved public health surveillance, better-informed policy creation, and enhanced capabilities to respond to mass fatality incidents. Ultimately, these measures will contribute to the well-being of communities and assist public health prevention efforts.
The Model Postmortem Examinations Act, created by the National Conference of Commissioners on Uniform State Laws in 1954, outlined a state medical examiner system, allowing states to modify the model to fit its jurisdictional needs, though most states have not followed the Act’s suggestions. The overseeing body is now referred to as the Uniform Laws Commission, and no changes have been made despite multiple attempts for review requested by the National Association of Medical Examiners. The National Commission on Forensic Science recommended drafting a new model of medicolegal death investigation legislation to support states in improving their medicolegal death investigation frameworks and death investigations themselves. The Commission voted overwhelmingly to adopt the recommendation in January 2017, though no action has been taken by the Attorney General to date. While it is unlikely a national framework will be adopted by all states, model legislation for medicolegal death investigation systems can allow states to adjust the legislation to best fit their needs while maintaining a minimum standard.
Excited Delirium: A Fatal Term Laid to Rest
Excited delirium, a diagnosis generally characterized by a severely agitated state, made headlines in some of the most contentious deaths in custody, including being mentioned by an officer as a concern when George Floyd was in a prolonged prone position. Law enforcement officers have been trained to recognize excited delirium as a medical emergency requiring immediate medical intervention when someone shows extreme agitation, incoherent speech, increased pain with decreased sensitivity to pain, confusion or rapid changes in emotion, and muscle rigidity. Once the person is in custody or restrained, training outlined putting the person into the recovery position to avoid positional asphyxiation and awareness that sudden death can occur after a violent struggle. Autopsies in excited delirium cases generally reveal lung and brain swelling coupled with heart disease and recent cocaine use without providing a direct cause of death. The lack of clear signs of death during an autopsy requires forensic pathologists to relate known circumstances to the cardiovascular collapse.
History of a Controversial Term
The controversy around the use of excited delirium as a cause of death is that it was not formally recognized as a distinct medical diagnosis by many of the top medical associations, including the World Health Organization, the American Medical Association (AMA), and the American Psychiatric Association. The disputable cause of death has never been formally recognized in the Diagnostic and Statistical Manual (DSM), a guide to symptom diagnosis for mental health conditions, or the International Classification of Diseases (ICD), a guide to diseases and conditions to assist with classification and statistics tracking published by the World Health Organization. The lack of an ICD code dramatically reduces the ability to track the diagnosis in fatal and non-fatal circumstances. The American College of Emergency Physicians was the only medical organization that formally supported the diagnosis of excited delirium and its clinical use. The ACEP confirmed their support for the excited delirium diagnosis in 2021 and formally retracted their support for using the terminology in April 2023. The National Association of Medical Examiners does not endorse the use of excited delirium as a cause of death and recommends using underlying causes of the suspected delirium as the cause of death.
The history of excited delirium was first noted in the 19th century with the term delirious mania, with someone suffering from hyperactivity, psychosis, and sudden collapse. Other psychiatrists across the world added to the body of research and changed the mania phraseology, with excited delirium being coined in 1985 by an American forensic pathologist and psychiatrist to describe a person with superhuman strength, extreme fear and paranoia, hyperthermia, agitation, and generally involving recent cocaine use. Through the eyes of a forensic pathologist, there was no specific anatomic cause of death but a process of ruling out causes of death, such as in sudden unidentified infant death syndrome. In their seminal work, Drs. Welti and Fishbain reviewed seven case studies with cocaine involved with all and the decedents being hyperactive, violent, yelling, and thrashing around. Six of the seven case studies had increased strength, and all required restraints to reduce the violence. A 1998 review of 21 excited delirium deaths in Ontario, Canada, showed that all cases involved restraint for violence and hyperactivity with 18 people being in the prone position and three having pressure placed on their necks at the time of death, suggesting that the position of restraint may be directly related to the death and not the excited delirium itself. At least 166 deaths in police custody from 2010-2020 were attributed to excited delirium across the nation, though required reporting through the 2013 Death in Custody Reporting Act is complicated with data collection and antiquated reporting mechanisms.
The AMA noted that excited delirium was not a supported medical diagnosis and condemned the potential recognition of excited delirium as the sole reason for law enforcement officers to use excessive force. The AMA recognized that excited delirium has been disproportionately used in diagnoses for in-custody deaths of underrepresented minorities and misused to justify police actions. The 2021 policy also recommended utilizing non-law enforcement practitioners for de-escalation efforts and appropriate medication intervention, further recognizing racism as a threat to public health. One of the physicians who coined the term excited delirium completed a review of sex workers with a recreational drug use history and suggested that the deaths were due to a variant of excited delirium. All of the sex workers were Black women, and exhumations of some decedents after the forensic pathologist’s cause of death attribution to excited delirium was incorrect as the decedents were strangled to death, later leading to the arrest of a serial killer.
Citing Proper Cause of Death Classification
California banned the use of an excited delirium diagnosis as a cause of death, in medical treatments, police reports, and court proceedings. Assembly Bill 360 updated the California Evidence Code to state that excited delirium is not a valid cause of death or medical diagnosis but that descriptions of behavioral signs and symptoms can be stated in police reports and civil actions. The bill was signed into law in October 2023, marking the first state in the union to restrict the use of excited delirium. Some law enforcement agencies in California, in advance of the ban, removed the controversial term from policies and training material to focus on racial equity. Colorado’s Peace Officer Standards and Training, a law enforcement certifying board, will be removing excited delirium from law enforcement training starting on January 1, 2024. The updated training curriculum will focus on providing care to subjects in custody and requesting appropriate levels of care.
While the banning of the term excited delirium is logical based on its history and unsupported medical research, there are concerns about the government restricting medical professionals from being able to properly diagnose and classify their work. The Texas Governor signed HB 6 into law in June 2023, classifying all opioid toxicity-related deaths as poisonings to allow for homicide charges against those who manufacture and sell illegal drugs. California had its first successful prosecution of a drug dealer who sold a fentanyl-laced pill to a decedent in August 2023. However, there is no evidence that prosecutions for drug toxicity-related deaths are a deterrent to drug use or save lives. Texas did not pass the legalization of fentanyl test strips, allowing people to test their drugs for the presence of fentanyl prior to ingestion. Dictating exact wording for death certificates, such as “fentanyl poisoning” for opioid-related deaths may be the start of a slippery slope for laws restricting medical expertise and diagnoses.
History has been made to bar the use of excited delirium in medical and law enforcement settings, though recognizing medical and psychiatric emergencies is vitally important for the person in crisis to receive appropriate treatment. When someone shows signs of extreme agitation, incoherent speech, confusion, and paranoia, activating the emergency 9-1-1 system is essential to reducing mortality. Law enforcement officers should follow appropriate policies and procedures for deescalating and obtaining immediate care and referrals to mental health professionals to increase survival and recovery through crisis events.
Training for Safety and Success: Research & National Minimum Training Standards for Law Enforcement
Summary
Law enforcement is a highly visible profession where, without effective training, safety is at risk for both law enforcement officers and community members. Officers regularly respond to calls for service with uncertain risk factors and must balance the work with proactive activities to improve community well-being. Nationally, mandated training hours for new law enforcement officers are consistently less than those required for cosmetology licensure, with training quality and requirements varying significantly by state. Nearly three-quarters of states allow officers to work in a law enforcement function before completing the basic academy. Public trust and safety are placed in the hands of law enforcement officers, even if they lack the training, skills, and knowledge to be successful. Policing practices are regularly shaped by failures shown in national media, yet the shift in practices is rarely institutionalized in basic training practices.
To make communities safer and law enforcement officers more successful, the Biden-Harris Administration should fund research on the effectiveness of law enforcement training and create a national minimum standard for entry-level academy training to further support the Safer American Plan. The 2022 Executive Order on Advancing Effective, Accountable Policing and Criminal Justice Practices to Enhance Public Trust and Public Safety focuses on strengthening trust between communities and law enforcement officers, including training and equitable policing. The Department of Justice should oversee this research, and the Departments of Homeland Security, Labor, and Commerce can help create national standards and minimum training recommendations. Based on the findings and using pedagogical approaches for the most productive learning, minimum national training standards will be recommended by an interdisciplinary federal task force. Training can be used to compel change in law enforcement, improve community-police relations, and reduce liability while advancing community safety.
Challenge and Opportunity
Law enforcement actions have widespread implications due to the immense power and inherent risks associated with the position. The profession is plagued with complexity and unpredictability, further challenged by extensive discretionary capabilities and varied training requirements. Basic academy training is the foundational coursework for learning about laws and ethics, technical skills relating to actionable law enforcement functions, soft skill development, and honing critical thinking during stressful situations. However, more focus is placed on didactic portions with practical exercises than on cognitive, emotional, and social skills, which can be used to safely de-escalate situations. Even with these known training insufficiencies, academy training topics and hours are rarely updated. Training requirements and pedagogical approaches administered by peace officer standards and training or similar overseeing bodies generally require legislative updates to update curriculum standards, taking significant time and resources to enact change.
Back in 2015, President Obama highlighted the need for training and education in the 21st Century Taskforce on Policing, citing that law enforcement officers (LEOs) are required to be highly skilled in many operational areas to meet the wide variety of challenges and increasing expectations. The Biden-Harris Administration has vowed to advance effective, accountable policing through the Safer America Plan, noting that change at the local and state level requires congressional action. The Safer American Plan would provide funding for 100,000 additional LEOs, all of whom will require training to be effective in their role. Academy training requirements are not regularly collected or monitored at the federal level, and research is not routinely completed to show the efficacy of the training provided. The lack of data on law enforcement actions further complicates the training process, as the time spent during patrol is not regularly cataloged and reviewed to determine where officers spend most of their time. Data showing where officer time is spent can guide training decisions and adjust hours to provide skills for the most commonly utilized skill sets.
There is no national training standard for LEOs: state requirements vary from 1345 hours in the basic academy in Connecticut to 0 hours in Hawaii. The basic academy provides future LEOs foundational knowledge and skills in law, defensive tactics, report writing, first aid, communication, and other critical skills. The average length of basic training is 833 hours, with an average of 73 hours dedicated to firearm skills and 18 hours to de-escalation techniques. While firearm familiarization and skills are of utmost importance due to the fatal consequences of not understanding the weaponry and one’s ability, the discharge of a firearm occurs significantly less than de-escalation and other communication techniques. When not used regularly, skills become perishable, and the lack of regular training on topics like firearms and traffic stops can reduce an LEO’s efficiency, response time, and safety. The 2022 Executive Order on Advancing Effective, Accountable Policing mandates training federal LEOs with clear guidance on use-of-force standards and implicit bias, but these basic tenets of policing requirements are not extended to state and local law enforcement.
Thirty-seven states allow LEOs to work before they have completed a basic training academy. The time LEOs can work before receiving basic training ranges from 3 months in West Virginia to 24 months in Mississippi. There are obvious dangers to LEOs and the public by providing a uniform and firearm to an untrained person to interact with the community in a position of power. Figure 1 shows the ranges of when the basic academy is required of new LEOs.
With the basic academy averaging 833 hours, or about 21 weeks, it may seem like a sufficient timeframe to train new law enforcement officers. However, it commonly takes at least six months to master a new skill, with the academy requiring many new skills to be developed simultaneously. The minimum basic academy hour requirement in California is 664 hours, though the training is commonly over 1000 hours. By contrast, earning a cosmetology license in California has more extensive hour requirements than the basic police academy, with cosmetology and barber training requiring 1000 hours for state licensure. While injuries can occur in cosmetology, the profession is inherently safer for the practitioner and the client.
FBI Director Wray noted a 60% increase in murders of law enforcement officers in 2021, explicitly noting that violence against law enforcement officers does not receive as much attention as it should. Of the 245 LEOs who died in the line of duty in 2022, 74 were feloniously killed, up from 48 in 2019. In 2022, 1194 people were killed by LEOs, with 101 people being unarmed. Black people are disproportionately killed by LEOs, at nearly triple the population rate. The statistics of community members killed do not differentiate between legally justified uses of force and illegal actions, so a true picture of potential training concerns versus ethical violations cannot be determined.
Recognizing the insufficiencies of current LEO training raises opportunities for data-driven improvements. Research is needed to determine the efficacy of the basic academy training in each state, with comparisons made to provide an overall recommendation for minimum national standards. Innovation should be encouraged when developing future training standards, as the basic academy training has not embraced technology or newer learning techniques that may aid in practical decision-making and skill mastery.
Plan of Action
Training can be used to implement vital reforms in law enforcement, potentially saving lives. A multipronged, transparent approach is needed to determine the efficacy of current training before introducing innovation and minimum training standards. Multiple agencies will need to collaborate to complete the evaluation and create recommendations to incorporate inclusive views through multifaceted lenses and coordinate future actions. Transparency of the research and its goals, including making findings available on public-facing websites, is needed for accountability and to foster trust in the process of improving law enforcement. Additional detail of the proposed agencies and their roles is below.
Recommendation 1. Fund research for current LEO training and efficacy
Before overhauling training, data is needed to provide a baseline of training in each state, including its perceived efficacy by stakeholders. The DOJ should create and administer competitive grants to evaluate current training in every state/territory and complete surveys, interviews, and focus groups with stakeholders to determine the impact of training. Use-of-force incidents, accidents, LEO decertification, and other aspects of potential training deficiency should be examined for additional insight into effectiveness.
Research should also be conducted on fatal and accidental duty-related incidents to determine the human and other contributing factors. Data and trends gained from the research should be incorporated into minimum training standards to reduce future errors. Competitive grants can be provided to evaluate potential root causes of duty-related fatal and accidental deaths.
A key component of the research phase will be bringing the researchers together to discuss findings, regional and national trends, and recommendations. Creating a formal networking process will allow for best practices to be shared across all states/territories participating and made available to all LEO training commissions.
Recommendation 2. Spark innovation from adult learning experts and practitioners for LEO training
Through a competitive grant process, the DOJ’s Office of Justice Programs can advertise funding opportunities and outline the application process. Grants focusing on practitioners and adult learning experts in collaboration, potentially through practitioner-higher education partnerships, can assist in bringing the necessary experience from the field and adult learning. Curriculum designers should consider immersive or simulation training experiences and the use of technology in training. In addition, they should consider redesigning the rigid paramilitary format to encourage LEOs to utilize critical thinking skills, improve adaptability, and hone communication skills. Using Challenge.gov can also provide additional insights from the community.
Recommendation 3. Create national minimum standards for LEO basic academy training
Using the recommendations from the state law enforcement training researchers, the fatality factor researchers, practitioner and adult learner experts, FLETC, and DOL, a compilation of recommendations from NIST, DOJ, DHS, DOC, and DOL of national minimal standards should be completed. Requirements for academy instructors will also need to be established, including training program requirements and regular reviews of their performance and impact. NIST will use the information gathered, including contemporary training topics and a focus on adult learning techniques, and create a draft standard. The research teams and the public will have an opportunity to comment on the draft standards, then NIST will adjudicate the comments before sending the standards to an SDO for additional feedback for a quality, peer review.
The DOJ’s Office of Justice Programs will offer grants to all interested state LEO training bodies to adhere to the national minimum standard, with funding for planning, Implementation, and evaluation of the project. Grants should require a three-year timeline for implementation to ensure trainees receive training before their first day on the streets and the basic academy meets the minimum national requirements.
Recommendation 4. Evaluate curricula changes with environmental changes
Grant funding for the planning and implementation should extend an additional two years for the evaluation component. Evaluators chosen during the grant process can review how well training adheres to the national standards across all academies in the state, LEO feelings of preparedness upon graduation and quarterly after that for up to two years, and supervisor/administrator feedback on LEO performance after the academy. Deidentified records of unjustified use-of-force, decertification, and criminal actions can be reviewed for additional insight into the effectiveness of the basic academy training.
An overall program evaluation will be needed, including reviewing the state evaluations and the overall administration of the project. The grant can be open to one organization or multiple organizations with the selection and funding provided by DOJ’s Office of Justice Programs. Competitive grant funding for up to $5 million should be awarded for the six-to-eight-year evaluation.
Budget Proposal
A budget of $125 million is proposed to evaluate current LEO training, develop minimum requirements, and evaluate the implementation. The primary research of determining current LEO basic academy training and efficacy requires $500,000 for one researcher/research group per state/territory, totaling $28 million.
For the adult learning and practitioner component, competitive grants for up to 10 collaborations should receive up to $300,000 each, totaling $3 million. FLETC and DOL can be funded for their participation in the minimum standard creation at $1 million each, totaling $2 million.
Each state LEO training commission should be eligible to receive up to $2 million each to plan, implement, and evaluate the minimum training standards. If all states/territories participate, the funding will total $112 million.
An evaluation of the entire program will be conducted for $5 million for six to eight years of expected evaluative work. The final report will be provided to the DOJ to determine if performance metrics were met.
Conclusion
The national LEO training standard is meant to be the floor of training for states and does not remove the oversight of state peace officer training commissions. Every LEO should go through a basic academy and field training before serving the community to ensure they can be safe and effective in their roles. Developing innovating training techniques can help increase skills and understanding of vital topics while refining critical thinking skills in high-stress situations. Minimum training standards can improve safety for the public and first responders, reduce ethical and criminal violations by LEOs, and assist in repairing community-police relationships.
No. The 10th Amendment restricts the federal government from mandating standards, but federal grant funding can be restricted from states that do not meet the minimum training mandates. Precedence was made with DOJ’s Community Oriented Policing Services grants, which restrict federal funding if the agency’s use-of-force policy does not adhere to federal, state, and local laws.
States can update their training requirements at their will. States may be incentivized with federal grant funding, rather than waiting for unfunded and underresourced local attempts. Change involving many or all states can create pressure to conform to minimum requirements where there is currently little pressure with no financial incentives offered.
In December 2022, the House passed S.4003 Law Enforcement De-Escalation Training Act of 2022. The bill provides $34 million to the Department of Justice to fund scenario-based training for de-escalation and use-of-force for individuals experiencing a mental, suicidal, or behavioral crisis.
Stemming from the deaths of two unarmed Black men, HR 1280 and HR 1347 requested additional training and standards to reduce excessive force by LEOs. HR 1280 passed the House, and HR 1347 was introduced to the House with no actions since 2021.
LEO training in the United States is among the lowest in the world, with France training LEOs for 10 months or 1600 hours, Scotland’s basic training lasting for 92 weeks or 3680 hours, India for 2.5 years or 5400 hours, and Finland for three years or 6240 hours, with an additional year of field training.
Most states require continuing education or professional development. Hawaii has no LEO training requirements, and New Jersey law states agencies may provide in-service training without hourly requirements. Once minimum standards for basic training are implemented, national minimum mandatory annual continuing education or professional education can be developed.
The first recommendation requests funding to assess and determine the current efficacy of law enforcement training in every state. The multistage research would include interviews, surveys, and focus groups with stakeholders to determine training perceptions and impact, while a comparison is made using data from use-of-force incidents, officer decertification, accidents, fatal incidents, and other areas of potential training deficiency.
Health Care Coverage for the Incarcerated Population to Reduce Opioid-Related Relapse, Overdose, and Recidivism Rates
Summary
Untreated substance use disorders (SUDs) are common among those who pass through the criminal justice system. At both the state and federal levels, re-entry into communities is a critical time period for these individuals. Preventing opioid relapse and potential overdose post-release can prevent recidivism, and improve an individual’s life after time in jail. Medication-assisted treatment (MAT) for opioid use disorders (OUDs) can help some sustain recovery. However, there are many barriers that interfere with the distribution of medication: cost, accessibility, and distribution are difficult to overcome, along with a lack of professionals trained to prescribe medication for OUDs.
To address this facet of the growing opioid crisis, the United States Department of Justice (DOJ) and the Centers for Medicare & Medicaid Services (CMS) should facilitate the accessibility for medications for OUDs (MOUDs) and train professionals to prescribe MOUDs. Additionally, incarcerated individuals with an OUD should have intensive case management that continues through reintegration into society. Finally, Medicare coverage should be available in order to continue treatment and support successful reentry into their community. Together, these will help reduce risks of recidivism, opioid-related relapse, and overdoses during reintegration back into their community.
Challenge and Opportunity
Approximately 65% of the United States prison population has a substance use disorder. An estimated 17% of those detained in state and federal prisons who meet the criteria for substance use disorder have an opioid use disorder specifically. Repeated drug usage causes a person to grow physiologically reliant on the drug, requiring more to have the desired effect, known as increasing tolerance. Individuals with an OUD lose their tolerance to the drug while incarcerated, which sets them at a greater risk of overdose mortality upon release. The risk of mortality from a lethal overdose is more than 12 times greater than that of another person within two weeks of being released from jail or prison. A meta-analysis determined that MOUDs during incarceration increased post-release treatment involvement and reduced opioid use post-release. Similarly, a randomized control trial at a Baltimore pre-release prison setting, showed that those who began methadone therapy and counseling while in prison were more likely to continue treatment post-release. They also had reduced rates of opioid use re-offending over the course of six months compared to those who received counseling only.
Methadone, buprenorphine, and naltrexone are MOUDs that have been authorized by the Food and Drug Administration for the treatment of OUDs. Research on the utilization of MOUD has demonstrated to be an effective treatment, specifically with methadone and buprenorphine. However, the distribution amount of MOUDs in the criminal justice system settings is low: only 3.6% of incarcerated individuals with OUD across the United States were prescribed and administered buprenorphine. According to the Pew Charitable Trusts and Substance Abuse and Mental Health Services Administration (SAMHSA), just 14 states administered at least one MOUD, 39 states provided naltrexone in jail or prison settings, and only one state (Rhode Island) provided all three MOUDs. Increasing the percentage of MOUD administration in carceral settings and after release across the United States is critical in order to reduce opioid overdose deaths.
Rhode Island’s Approach to Opioid Use Disorder Treatment
The Rhode Island Department of Corrections (RIDC) is the first correctional system to launch an extensive program to screen individuals for an OUD upon entry, offer all three MOUDs to eligible incarcerated individuals, and continue with treatment post-release. The RIDC MAT program provides incarcerated individuals with access to MOUDs, and counseling during incarceration. RIDC MAT also provides linkage to care after release through a partnered non-profit organization, Community Organization for Drug Abuse Control (CODAC) Behavioral Healthcare. Together, RIDC and CODAC have established a successful pipeline for the continuation of MAT post-incarceration. Prior to an individual’s release date, CODAC develops a re-entry strategy with the assistance of case management and care providers. As a result, Rhode Island’s statewide overdose fatalities decreased by 12% in the first year of this program’s adoption, while post-incarceration overdose deaths decreased by 61%. A decrease in mortality rates related to opioid overdose post incarceration allows approximately $7,300 more in personal income per individual’s extended years of life. Other states have turned to Rhode Island’s MAT program to learn from and advocate for incarcerated individuals in order to treat OUDs during and after incarceration, and help reduce recidivism.
Challenges for Implementation
Despite these strong results, challenges remain.
Opioid use treatment and services are covered by health insurances under the Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008. However, incarcerated individual healthcare coverage is entirely operated by the state, which contributes to the above mentioned disparities in drug therapeutic access and counseling–but only while incarcerated. As individuals transition back into society, if they do not have health insurance to pay for their MOUDs or other rehabilitation treatments, they lose treatment, and experience an increased likelihood of relapse.
The Medicaid Inmate Exclusion Policy under the Social Security Act prevents and prohibits Medicaid coverage while incarcerated, making it difficult for formerly incarcerated individuals to acquire healthcare upon release, and thus access MOUDs. The majority of these individuals qualify for Medicaid upon release since they are low-income and fall below the federal poverty line. In 2018, Congress provided waiver opportunities for CMS to connect individuals who were recently released from jail/prison to healthcare across the states, but not federally.
Medicaid Section 1115 Waivers
To combat this gap, states are waiving the Medicaid Inmate Exclusion Policy to provide Medicaid coverage for incarcerated individuals upon release by filing Section 1115 waivers. A section 1115 waiver is a provision within the Social Security Act that grants the Secretary of Health and Human Services the authority to waive specific requirements within the Medicaid program. Section 1115 waivers offer states the flexibility to design and implement innovative approaches to enhance access to healthcare. To obtain approval, states must submit proposals outlining their proposed changes and demonstrate that the waiver will not increase federal government expenditures over the waiver period. Once approved, the waiver permits the states to operate the Medicaid program with modified, exempted, or alternative requirements. For instance, Section 1115 waivers from New Hampshire and Utah were approved, enabling the expansion of healthcare coverage to incarcerated individuals. Under the waiver, incarcerated individuals are granted full Medicaid coverage for care coordination and provider services, which commences approximately one month prior to their release.
Plan of Action
The Biden Administration has urged states to submit Section 1115 waivers to propose options for expanding coverage in order to reduce health disparities, remove barriers to MOUDs treatment access, and find long-term solutions to OUDs issues. It is imperative that the federal government prioritize reducing relapse, and opioid overdose mortality rates during incarceration and post-release in order to reduce recidivism. The DOJ, CMS, and SAMHSA should collaborate to develop a pipeline that expands training across professionals, have MOUDs more accessible to correctional facilities, and have healthcare coverage post-release.
Recommendation 1. Compare and contrast the Section 1115 waivers submitted by states to encourage and detail advantages to the remaining states.
A root of the issue is the failure to provide pre-release healthcare coverage to incarcerated individuals in order for them to continue having coverage post-release. Hence, increasing the access to healthcare post-release by states applying for Section 1115 waivers to propose measures and assist incarcerated individuals in obtaining healthcare coverage is important. Currently 35 states have filed approved Section 1115 waivers. Collecting data on these states would provide insight into how these waivers reduce recidivism and overdose rates. The Agency for Healthcare Research and Quality (AHRQ) should issue an open call for evidence synthesis to delve into the impacts of Section 1115 waivers. By doing so, AHRQ would aim to conduct a comprehensive analysis of the impacts and outcomes from the implementation of Section 1115 waivers. This initiative would contribute to evidence-based decision-making and further enhance the understanding of the implication of Section 1115 waivers on healthcare. Examples of data collection that could be obtained to assess the success of Medicaid resources are:
- Overdose mortality rates between those who have Medicaid and those who do not
- Post-release drug-related opioid reoffending
- Economic impact such as quality-adjusted life years gained.
Once the data has been gathered, it is essential that the dataset is made publicly accessible to researchers. The dataset can be published on the CMS data website, enabling widespread access and utilization for researchers. This accessibility will allow researchers to examine the significance of reducing overdose-related fatalities after incarceration and assess how the expansion of Section 1115 waivers could contribute to achieve this reduction.
Recommendation 2. Increase opioid treatment program accessibility during and after incarceration.
Rhode Island’s MAT program has shown to be effective in reducing opioid overdose deaths. A replica of the Rhode Island program has improved OUD treatment to reduce opioid related relapses and death in a correctional facility in Massachusetts. In order to provide intensive case management when individuals come into contact with the criminal justice system and adequately rehabilitate them, correctional facilities should use a method similar to that used by Rhode Island’s Department of Corrections MAT program. Since correctional facilities and licensed professionals must be accredited by the DEA and SAMHSA to provide MOUDs, individuals will have the opportunity to have access to MOUDs at Opioid treatment programs (OTPs) during and after incarceration who are certified. Thus, the DOJ and SAMHSA should collaborate with CODAC and similar organizations to increase OTP accessibility across correctional facilities during and after incarceration. These organizations can assist with creating a re-entry treatment plan during incarceration and continue after release. Incarcerated individuals will have access to MOUDs at OTPs as well as counseling. This aims to increase accessibility to MOUDs, licensed therapists, and medical doctors.
Recommendation 3. Intensive case management during incarceration should continue when reintegrating back into the community.
The DOJ, CMS and OTPs should further collaborate to establish a pipeline that aids individuals to combat OUDs. Currently, upon release, formerly incarcerated individuals’ MOUD treatment is terminated and they do not have access to treatment unless they are referred to a rehabilitation center or seen by a licensed professional. The first two weeks after release are crucial because there is a higher risk of relapsing. Thus, it is essential for correctional facilities to assist incarcerated individuals to apply for Medicaid within a few months of release to access MOUDs and therapy. Medicaid would cover MOUD costs and counseling services at OTPs or similar organizations. MOUD treatment should be administered during prison in order to commence proper rehabilitation, whether that is at a correctional facility or an OTP. Subsequently, continuing their pharmacological treatment in parallel with counseling post-release reduces relapse, withdrawal symptoms, and overdose deaths. This aims to expand access while in a correctional facility and continue treatment post-release to reduce opioid mortality rates.
Conclusion
Opioid relapses and overdoses following imprisonment have escalated significantly, accelerating the chance of overdose mortality. Incarcerated individuals with an OUD should get comprehensive case management while incarcerated that continues as they reintegrate into their communities. However, the Social Security Act prevents incarcerated individuals from receiving Medicaid coverage while incarcerated. Implementing these measures will decrease overdose mortality rates, risk of relapse, and reduce recidivism.
In Massachusetts, researchers were able to assess an estimated cost and benefits of administering MOUDs during incarceration, using the Researching Effective Strategies to Prevent Opioid Death (RESPOND) simulation model. The availability of all three MOUDs during incarceration showed that it was cost effective at approximately $7252 per quality-adjusted life year gained and reduced 1.8% of opioid related overdose deaths.
The U.S Department of Health and Human Services (HHS) has provided science and community-based approaches to combat the opioid epidemic crisis. In the past years, the HHS has allocated $2 billion in grants to help reduce opioid mortality and relapse rates across the United States. Researchers and community-based organizations can apply for grant money from HHS for data collection on how Section 1115 waivers have improved reducing recidivism and overdose rates.
The DOJ has approximately allocated $340 million in grant award funding money to battle the opioid crisis. $7.2 million dollars have been used to treat individuals with a substance use disorder and assist with support during incarceration and reentry services.
The United States is in the middle of an emerging life-threatening opioid epidemic crisis that is affecting over 33,000 deaths per year from prescription and synthetic opioids. The opioid epidemic crisis is highly prevalent among the criminal justice population. This impacts individuals across the country, not just in specific states. The federal government should encourage individual states to apply for federal funding that is available in order to combat the opioid epidemic crisis.
The use of MOUDs in OTPs in the United States is regulated by the 42 Code of Federal Regulations (CRF) 8. This regulation established a system for accrediting and certifying OTPs in order to grant the ability to dispense and administer FDA approved MOUDs. More information on the process of accrediting and certifying OTPs can be found in SAMHSA website.
Given the rigorous nature of the accreditation process, obtaining accreditation for OTPs can be an intricate process, which involves several steps and requirements, including: thorough assessments of program infrastructure, staff qualification and training, and compliance with regulatory standards. These factors collectively contribute to the length of the accreditation process, potentially deterring some facilities from pursuing OTP status. Another aspect to consider is the decision-making process of states regarding the application for Section 1115 waivers. One significant consideration revolves around funding and financial considerations. States often conduct an extensive evaluation to assess the potential financial implications and cost-sharing arrangements associated with the Section 1115 waiver before finalizing their decision to apply. Despite these challenges, it is crucial to acknowledge that implementing OTP accreditation and Section 1115 waiver approvals play a crucial role in reducing relapse rates post-incarceration, while also creating a more comprehensive and effective healthcare system that saves lives by addressing the opioid crisis and minimizing recidivism.
Let’s Talk About Death: The State of Medicolegal Death Investigations
We will all die. But generally, people don’t like talking about it, and fewer people want to make the details of death their actual job. Accurate death reporting, however, is necessary for public health surveillance, timely health interventions, and reduction in avoidable deaths. Forensic pathology, a medical sub-specialty that focuses on performing autopsies to determine the cause of death, has been popularized and glamorized through popular television shows without showing the dire shortage of forensic pathologists in the United States.
Approximately 750 forensic pathologists are currently practicing, who have significantly higher workloads due to the opioid epidemic and other career challenges, such as being in an administrative role in a Medical Examiner’s Office. Even with medicolegal death investigative offices often portrayed in popular entertainment as fully staffed and without case backlogs, the existing system is stressed with many variations in structure that do not lend to a standardized national death investigative system. Funding for essential office services, training, accreditation, and supporting physicians to train as forensic pathologists are needed to improve the current systems and provide accurate causes and manners of death.
The medicolegal death investigation system in the United States varies by state, with multiple office types utilized. Popular television and media commonly use ‘coroner’ and ‘medical examiner’ interchangeably, though their formal definitions vary quite significantly. State and county charters generally dictate the type of medicolegal death investigation system in place, with some states utilizing a state-wide system, such as Arkansas. In contrast, other states have a mix of systems that vary by county. There are approximately 2000 medicolegal death investigative offices nationally, employing just under 11,000 full-time employees.
A coroner is an elected or appointed department head responsible for medicolegal death investigations and determining the cause and manner of death. Coroners are generally not required to have any medical knowledge or death investigation experience. A medical examiner is generally an appointed physician who is a department head. However, not all physicians must be board-certified forensic pathologists who conduct forensic postmortem examinations (autopsies). In some states, such as Wisconsin, medical examiners are not required to be physicians, yet the term is still utilized when a department head is appointed.
In California, there are two additional variations, including a Sheriff-Coroner system where the elected sheriff also serves as the coroner as in Orange County, and a Medical Examiner-Coroner system that is a separate appointed county entity in Santa Clara County. Texas has a Justice of the Peace elected position that hears traffic, misdemeanor, civil, tenant/landlord disputes, and truancy cases, in addition to completing death investigations. The requirements are to be a citizen of the United States, a resident of Texas for a year, registered to vote, and 18 years of age with no felony convictions. Despite the term ‘justice’ in the title, there is no requirement for law or investigative training to be elected into a Justice of the Peace role.
Only 16 states require training for coroners and medicolegal professionals. California has the most robust training requirement for medicolegal death investigators, with 80 hours of structured medicolegal death investigation-based training required within the first year of appointment. Justices of the Peace must complete 80 hours of training during their first year in office and 20 hours of training in the following years, though there is not a prescribed amount of medicolegal-focused training. Other states have vague wording such as “must obtain additional training in medicolegal death investigation” or rely strictly on on-the-job training. The lack of standardized basic training nationally lends itself to making mistakes, providing incorrect causes of death, incorrect identifications, and ultimately negatively affecting families of decedents.
Outside of different terminology for the roles, the function of medicolegal death investigations remains the same: identify decedents, notify the legal next of kin, collect evidence and property, and determine the cause and manner of death. Deaths that fall into the jurisdiction of a medicolegal death investigative office are considered unnatural, when the decedent has no known medical history, or a physician who saw the decedent as a patient cannot opine what may have caused an otherwise natural death.
Medicolegal death investigative offices make two determinations: 1) The cause of death, or what immediately led to the death and 2) The manner of death, a categorization of the cause of death and the known circumstances surrounding it.
The cause of death is what immediately led to the death and the sequence of events if there are multiple factors. The cause of death should be determined by a board-certified forensic pathologist in medicolegal death investigation cases. The manner of death is a categorization of the cause of death and the known circumstances behind the death. The manner of death can be natural, accident, suicide, homicide, or undetermined, and is generally determined by the agency’s administrator or a designee.
The cause and manners of death should be reached through an unbiased investigation and autopsy, as bias can lead to incorrect causes and manners of death with undesirable consequences to kin and public health records. The shortage of forensic pathologists leads to physicians working for multiple agencies, circumventing an accreditation standard of a forensic pathologist not completing more than 250 autopsies annually.
With the vital role of medicolegal investigative offices in public health, identification of decedents, and determining causes and manners of death, only 43% of medicolegal offices have a computerized case management system to track deaths and work completed. Also worrisome is that about 80% of agencies have access to the internet outside of their personal devices. The internet provides significant assistance in finding legal next of kin, adding unidentified person information to national databases, and communicating with stakeholders via email. Investigations were completed by internal agency employees about 85% of the time, and scene photography was completed by employees about 71% of the time. Less than 20% of agencies completed autopsies in their facility, with the vast majority of agencies contracting forensic pathology services outside of their jurisdiction.
State and local charters will make transitioning to a standardized national medicolegal death investigative system challenging, but appropriate funding can assist with providing fundamental resources for offices and improve training nationally. Accreditation of medicolegal death investigative offices can ensure that best practices and minimum standards are met, though the shortage of forensic pathologists will challenge accreditation viability. Certification of death investigators, which is not currently required nationally, encourages high ethical and investigative standards for practitioners and requires training, experience, and funds for earning certification. Nationally prescribed, foundational medicolegal death investigation training is needed to provide a basic knowledge level to all medicolegal personnel. This will lead to more accurate investigations and determinations of cause and manner of death. Through a collaborative effort of the federal government with local medicolegal agencies, death investigations can be improved across the United States to best serve families, communities, and the public health system.
Navigating Homelessness: The Effect of Housing Navigation Centers on Recidivism
Adequate resources, shelter, and opportunities for people to secure permanent housing are critical for alleviating homelessness and reducing recidivism rates.
The unhoused population faces many challenges in securing housing, especially if they are justice-involved or suffering from mental health or substance abuse disorders. The U.S. Department of Housing and Urban Development’s 2022 Annual Homelessness Assessment Report found that over 580,000 people were experiencing homelessness nationally, with 40% being unsheltered. There was a seven percent increase in sheltered homelessness from 2021 to 2022, possibly related to increasing housing capacity after COVID-19 restrictions. Unhoused persons are 514 times more likely to be arrested and charged with crimes when compared to the non-homeless population, and those who are released from prison have an average recidivism rate of 68% within three years. The cycle of crime and recidivism among unhoused persons can lead to significant challenges in receiving and maintaining permanent housing.
Promising policy tools like Housing Navigation Centers (HNC) are already showing great results. HNCs are a low-barrier intervention for unhoused populations to access services and focus on providing temporary housing while providing support to gain permanent housing. HNCs generally provide wrap-around services, including assisting with basic needs, case management, legal services, social services, career assistance, educational services, transportation assistance, mental health treatment, medical care, substance abuse treatment, and housing services.
California, which bears the brunt of the homelessness crisis (California holds 12% of the total US population but accounts for 30% of the nation’s homeless population and 50% of the unsheltered homeless population) has proved a great case study for the effectiveness of HNCs.
From 2019 to 2022, there was a 22% increase in homelessness in Alameda County, CA, with 16% of people surveyed citing the pandemic as a cause for their homelessness. San Francisco, just north of Alameda County, had 6858 people experiencing homelessness in 2017, with 8035 people in 2019 (17.2% increase), and 7754 people in 2022 (3.5% decrease from 2019).
In 2019, wanting to provide support for people experiencing homelessness, the City of Hayward, seated in Alameda County, bid for and received a nearly $1M grant to create an HNC, as well as train law enforcement on diversion, and provide wrap-around housing. The grant goals, part of a larger state effort to lower recidivism rates and mass incarceration, included coordinating wrap-around services with extensive case management, providing permanent housing, and reducing homelessness.
Across a three-year study conducted on the grant’s efficacy, 188 justice-involved individuals received housing at the HNC, and nearly 70% exited to permanent housing. Recidivism, defined as an arrest for a new felony or misdemeanor crime, was 9.6%, compared to an average recidivism rate of 68% within three years of release from prison.
Using the federal definition of recidivism, 0% of participants received a conviction for a new felony or misdemeanor throughout the evaluation period, though some of this was due to pandemic-related changes in policing practices and COVID-19’s effect on slower court proceedings. The point-in-time count reflected a 21.8% decrease in homelessness in Hayward, despite a 21.5% increase in homelessness in Alameda County from 2019 to 2022, showing the HNC’s potential impact. A similar study in Los Angeles confirmed that housing assistance with long-term placement assistance reduced recidivism by 20% over an 18-month period, with non-housing services having no effect on recidivism.
The U.S. Interagency Council on Homelessness aims to reduce homelessness by 25% by 2025, focusing on equity, data, and collaboration. The solutions include housing and support services, and HNCs would be positioned to fulfill both of these roles.. As grant and private funding remain available, cities and jurisdictions should utilize HNCs to assist in reducing homelessness and recidivism while improving the quality of life for community members.
The Ghost Guns Haunting National Crime Statistics
There are over 350 million guns in the United States, and an unknown number that are completely untraceable. The proliferation of privately made firearms, also known as ghost guns, has contributed to the highest rate of firearm-related homicides in 25 years. Non-serialized and inexpensive, ghost guns have emerged as a cataclysmic issue in the violence epidemic in our nation.
In his 2022 State of the Union address, President Biden outlined a comprehensive gun strategy that included an effort to help stop the propagation of ghost guns. Eleven states have adopted regulations for ghost guns, though much more is needed to curb the current grave issues with these types of firearms. Federally-approved standardized training needs to be provided to law enforcement officers so they can properly identify unserialized weapons. Law enforcement agencies need to update case management systems to allow for the real-time tracking necessary to determine ghost gun involvement in crimes and how laws and enforcement efforts are curbing their use.
Without serial numbers or other traceable features on the gun frame, slide, or other components, tracking weapon movement from sales and thefts is impossible. Casings recovered from shooting scenes can be tracked nationally through the National Integrated Ballistic Information Network, utilizing the individuality of firing pins on casings and linking casings from different scenes to one weapon. Even with tracking capabilities from casings, ghost guns create significant investigative and safety challenges, especially since most of the ghost weapons authorities are able to seize are possessed by persons prohibited from owning a firearm.
Unlike commercially-made serialized firearms, ghost guns circumvent traditional background checks, convicted felon restrictions, and waiting periods since they are sold as components rather than a completed gun. Some components of ghost guns can also be 3-D printed with readily available online instructions, or milled, where tools are used to drill weapon components. After being denied a traditional firearm purchase two years earlier, a 23-year-old obtained parts and instructions and built a ghost gun, later using the weapon to kill five people in Santa Monica, CA.
Ghost guns are not new, with assembly kits being available since the 1990s. The increasing ease of internet sales has made obtaining the weapons easier than ever. The component nature of the assembly kits allowed firearms sellers to capitalize on legal loopholes by selling unfinished receivers for assault-style rifles, bypassing the ban on assault rifles in California and other states. Ghost guns are sought after by violent extremists, felons, and persons prohibited from legally possessing firearms.
There have been over 37,000 ghost guns recovered since 2017, with a 1083% increase in recoveries from 2017-2021. The recovery of these firearms is likely underreported, with many law enforcement agencies not having the reporting tools or training required to recognize and trace unserialized weapons. Recognizing the dangers of ghost guns and their unrestricted nature, the Biden Administration has supported new laws to serialize existing and future privately made firearms, require background checks for gun kit purchases, and require manufacturers to be federally licensed. The Bureau of Alcohol, Tobacco, Firearms, and Explosives also redefined gun components in April 2022 to be more inclusive of the new types of weapons produced and require serialization of vital components.
Ghost guns continue to be one of the biggest challenges to fighting gun violence. An increase in training law enforcement officers to recognize and adequately track ghost guns will assist in data collection, and priority should be placed on ensuring compliance with new laws. As technology changes and other firearm-type components emerge, the government must remain apprised of future threats to public safety and provide resources to research this phenomenon and reduce the danger to the community.
We have the data to improve social services at the state and local levels. So how do we use it?
The COVID-19 pandemic laid bare for some what many already knew: the systems that our nation relies upon to provide critical social services and benefits have long been outdated, undersupported, and provide atrocious customer experiences that would quickly lead most private enterprises to failure.
From signing up for unemployment insurance to managing Medicaid benefits or filing annual tax returns, many frustrating interactions with government services could be improved by using data from user experiences and evaluating it in context with similar programs. How do people use these services? Where are customers getting repeatedly frustrated? At what point do these services fail, and what can we learn from comparing outcomes across different programs? Many agencies across the country already collect a huge amount of data on the programs they run, but fall short of adequately wielding that data to improve services across a wide range of social programs. Evaluating program data is necessary for providing effective social services, yet local and state governments face chronic capacity issues and high bureaucratic barriers to evaluating the data they have already collected and translating evaluation results into improved outcomes across multiple programs.
In a recent paper, “Blending and Braiding Funds: Opportunities to Strengthen State and Local Data and Evaluation Capacity in Human Services,” researchers Kathy Stack and Jonathan Womer deliver a playbook for state and local governments to better understand the limitations and opportunities for leveraging federal funding to build better integrated data infrastructure that allows program owners to track participant outcomes.
Good data is a critical component of delivering effective government services from local to federal levels. Right now, too much useful data lives in a silo, preventing other programs from conducting analyses that inform and improve their approach – state and local governments should strive to modernize their data systems by building a centralized infrastructure and tools for cross-program analysis, with the ultimate goal of improving a wide range of social programs.
The good news is that state and local governments are authorized to use federal grant money to conduct data analysis and evaluation of the programs funded by the grant. However, federal agencies typically structure grants in ways that make it difficult for states and localities to share data, collaborate on program evaluation, and build evaluation capacity across programs.
Interviews with leading programs in Colorado, Indiana, Kentucky, Ohio, Rhode Island, and Washington revealed a number of different approaches that state and local governments have used to build and maintain integrated data systems, despite the challenges of working with multiple government programs. These range of approaches include: adopting a strong executive vision, working with external partners (such as research groups and universities), investing in building up a baseline capacity that enables higher level analytic work, delivering crucial initial analysis that motivated policy makers to deliver direct state funding, and (most notably) figuring out how to braid and blend funds from multiple federal grant sources. The programs in these states prove that it is possible to build a centralized system that evaluates outcomes and impacts across a range of government services.
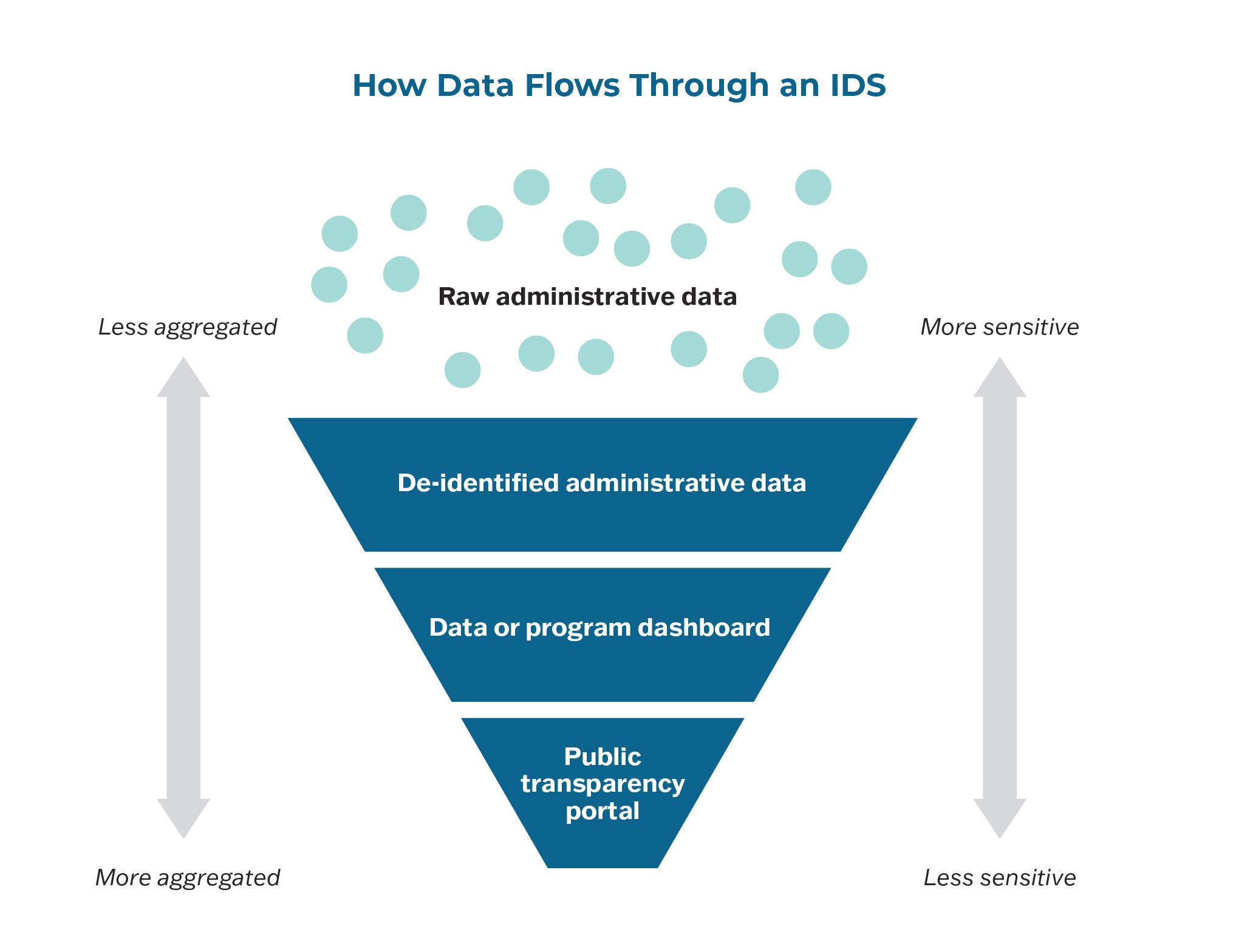
As data makes its way through an IDS, it is cleaned, verified, and matched with other data.
Stack and Womer lay out their menu of recommended options that states and localities can pursue in order to access federal funding for building data and evaluation capacity. These options include:
- stimulus funding from the American Rescue Plan’s State and Local Fiscal Recovery Fund and the Infrastructure Investment and Jobs Act;
- program-specific funding that funds centralized capacity;
- direct state or local appropriations;
- funding on a project by project basis;
- cost allocation billing plans; and
- hybrid funding models.
The authors advocate for states and localities to both blend funds and braid funds, when appropriate, in order to fully leverage federal funding opportunities. Blended funds are sourced from multiple grants but lose their distinction upon blending; this type of federal funding requires statutory authority, and may have uniform reporting requirements. Alternatively, braided funds also come from separate sources, but remain distinct within the braided pot, with the original reporting, tracking, and eligibility requirements preserved from each source. Financing projects and programs via braiding funds is far more time-consuming, but it does not require special statutory authority.
While states and localities can strengthen and expand integrated data systems alone, the federal government should also take important steps to accelerate state and local progress. Stack and Womer point out a number of options that do not require legislative action. For example, the Office of Management and Budget (OMB) and other federal agencies could issue clear guidance that recipients of federal grants must build and maintain efficient data infrastructure and analytics capacity that can support cross-program coordination and shared data usage. Regulatory and administrative actions like this would make it easier for states and localities to finance data systems via blending and braiding federal funds.
Integrated data systems are increasingly important tools for governments to achieve impact goals, avoid redundancy, and keep track of outcomes. State and local governments should take a page from Stack and Womer’s playbook and seek creative ways of using federal grants to build out existing data infrastructure into a modern system that supports cross-program analysis.