
Establishing an AI Center of Excellence to Address Maternal Health Disparities
Maternal mortality is a crisis in the United States. Yet more than 60% of maternal deaths are preventable—with the right evidence-based interventions. Data is a powerful tool for uncovering best care practices. While healthcare data, including maternal health data, has been generated at a massive scale by the widespread adoption and use of Electronic Health Records (EHR), much of this data remains unstandardized and unanalyzed. Further, while many federal datasets related to maternal health are openly available through initiatives set forth in the Open Government National Action Plan, there is no central coordinating body charged with analyzing this breadth of data. Advancing data harmonization, research, and analysis are foundational elements of the Biden Administration’s Blueprint for Addressing the Maternal Health Crisis. As a data-driven technology, artificial intelligence (AI) has great potential to support maternal health research efforts. Examples of promising applications of AI include using electronic health data to predict whether expectant mothers are at risk of difficulty during delivery. However, further research is needed to understand how to effectively implement this technology in a way that promotes transparency, safety, and equity. The Biden-Harris Administration should establish an AI Center of Excellence to bring together data sources and then analyze, diagnose, and address maternal health disparities, all while demonstrating trustworthy and responsible AI principles.
Challenge and Opportunity
Maternal deaths currently average around 700 per year, and severe maternal morbidity-related conditions impact upward of 60,000 women annually. Stark maternal health disparities persist in the United States, and pregnancy outcomes are subject to substantial racial/ethnic disparities, including maternal morbidity and mortality. According to the Centers for Disease Control and Prevention (CDC), “Black women are three times more likely to die from a pregnancy-related cause than White women.” Research is ongoing to specifically identify the root causes, which include socioeconomic factors such as insurance status, access to healthcare services, and risks associated with social determinants of health. For example, maternity care deserts exist in counties throughout the country where maternal health services are substantially limited or not available, impacting an estimated 2.2 million women of child-bearing age.
Many federal, public, and private datasets exist to understand the conditions that impact pregnant people, the quality of the care they receive, and ultimate care outcomes. For example, the CDC collects abundant data on maternal health, including the Pregnancy Mortality Surveillance System (PMSS) and the National Vital Statistics System (NVSS). Many of these datasets, however, have yet to be analyzed at scale or linked to other federal or privately held data sources in a comprehensive way. More broadly, an estimated 30% of the data generated globally is produced by the healthcare industry. AI is uniquely designed for data management, including cataloging, classification, and data integration. AI will play a pivotal role in the federal government’s ability to process an unprecedented volume of data to generate evidence-based recommendations to improve maternal health outcomes.
Applications of AI have rapidly proliferated throughout the healthcare sector due to their potential to reduce healthcare expenditures and improve patient outcomes (Figure 1). Several applications of this technology exist across the maternal health continuum and are shown in the figure below. For example, evidence suggests that AI can help clinicians identify more than 70% of at-risk moms during the first trimester by analyzing patient data and identifying patterns associated with poor health outcomes. Based on its findings, AI can provide recommendations for which patients will most likely be at-risk for pregnancy challenges before they occur. Research has also demonstrated the use of AI in fetal health monitoring.
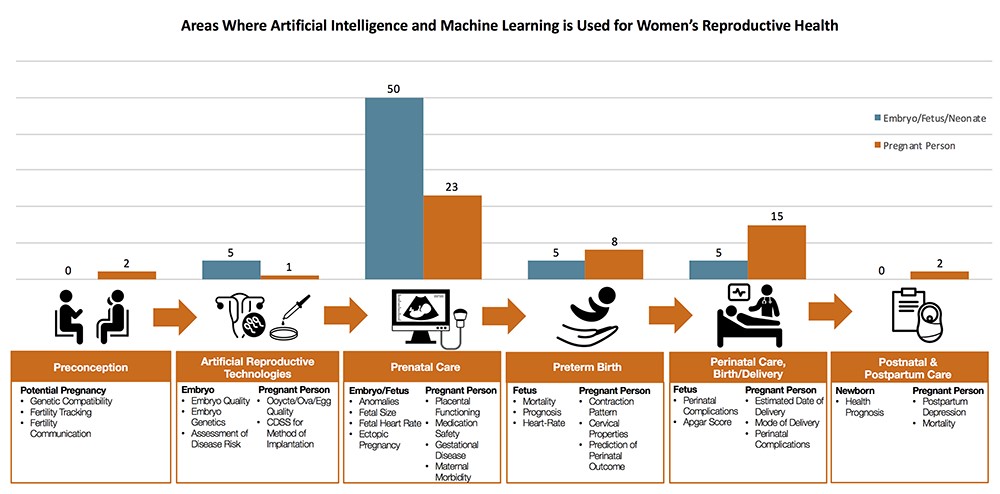
Source: Davidson and Boland (2021).
Yet for all of AI’s potential, there is a significant dearth of consumer and medical provider understanding of how these algorithms work. Policy analysts argue that “algorithmic discrimination” and feedback loops in algorithms—which may exacerbate algorithmic bias—are potential risks of using AI in healthcare outside of the confines of an ethical framework. In response, certain federal entities such as the Department of Defense, the Office of the Director of National Intelligence, the National Institute for Standards and Technology, and the U.S. Department of Health and Human Services have published and adopted guidelines for implementing data privacy practices and building public trust of AI. Further, past Day One authors have proposed the establishment of testbeds for government-procured AI models to provide services to U.S. citizens. This is critical for enhancing the safety and reliability of AI systems while reducing the risk of perpetuating existing structural inequities.
It is vital to demonstrate safe, trustworthy uses of AI and measure the efficacy of these best practices through applications of AI to real-world societal challenges. For example, potential use cases of AI for maternal health include a social determinants of health [SDoH] extractor, which combines AI with clinical notes to more effectively identify SDoH information and analyze its potential role in health inequities. A center dedicated to ethically developing AI for maternal health would allow for the development of evidence-based guidelines for broader AI implementation across healthcare systems throughout the country. Lessons learned from this effort will contribute to the knowledge base around ethical AI and enable development of AI solutions for health disparities more broadly.
Plan of Action
To meet the calls for advancing data collection, standardization, transparency, research, and analysis to address the maternal health crisis, the Biden-Harris Administration should establish an AI Center of Excellence for maternal health. The AI Center of Excellence for Maternal Health will bring together data sources, then analyze, diagnose, and address maternal health disparities, all while demonstrating trustworthy and responsible AI principles. The Center should be created within the Department of Health and Human Services (HHS) and work closely with relevant offices throughout HHS and beyond, including the HHS Office of the Chief Artificial Intelligence Officer (OCAIO), the National Institutes of Health (NIH) IMPROVE initiative, the CDC, the Veterans Health Administration (VHA), and the National Institute for Standards and Technology (NIST). The Center should offer competitive salaries to recruit the best and brightest talent in AI, human-centered design, biostatistics, and human-computer interaction.
The first priority should be to work with all agencies tasked by the White House Blueprint for Addressing the Maternal Health Crisis to collect and evaluate data. This includes privately held EHR data that is made available through the Qualified Health Information Network (QHIN) and federal data from the CDC, Centers for Medicare and Medicaid (CMS), Office of Personnel Management (OPM), Healthcare Resources and Services Agency (HRSA), NIH, United States Department of Agriculture (USDA), Housing and Urban Development (HUD), the Veterans Health Administration, and Environmental Protection Agency (EPA), all of which contain datasets relevant to maternal health at different stages of the reproductive health journey from Figure 1. The Center should serve as a data clearing and cleaning shop, preparing these datasets using best practices for data management, preparation, and labeling.
The second priority should be to evaluate existing datasets to establish high-priority, high-impact applications of AI-enabled research for improving clinical care guidelines and tools for maternal healthcare providers. These AI demonstrations should be aligned with the White House’s Action Plan and be focused on implementing best practices for AI development, such as the AI Risk Management Framework developed by NIST. The following examples demonstrate how AI might help address maternal health disparities, based on priority areas informed by clinicians in the field:
- AI implementation should be explored for analysis of electronic health records from the VHA and QHIN to predict patients who have a higher risk of pregnancy and/or delivery complications.
- Drawing on the robust data collection and patient surveillance capabilities of the VHA and HRSA, AI should be explored for the deployment of digital tools to help monitor patients during pregnancy to ensure adequate and consistent use of prenatal care.
- Using VHA data and QHIN data, AI should be explored in supporting patient monitoring in instances of patient referrals and/or transfers to hospitals that are appropriately equipped to serve high-risk patients, following guidelines provided by the American College of Obstetricians and Gynecologists.
- Data on housing from HUD, rural development from the USDA, environmental health from the EPA, and social determinants of health research from the CDC should be connected to risk factors for maternal mortality in the academic literature to create an AI-powered risk algorithm.
- Understand the power of payment models operated by CMS and OPM for novel strategies to enhance maternal health outcomes and reduce maternal deaths.
The final priority should be direct translation of the findings from AI to federal policymaking around reducing maternal health disparities as well as ethical development of AI tools. Research findings for both aspects of this interdisciplinary initiative should be framed using Living Evidence models that help ensure that research-derived evidence and guidance remain current.
The Center should be able to meet the following objectives within the first year after creation to further the case for future federal funding and creation of more AI Centers of Excellence for healthcare:
- Conduct a study on the use cases uncovered for AI to help address maternal health disparities explored through the various demonstration projects.
- Publish a report of study findings, which should be submitted to Congress with recommendations to help inform funding priorities for subsequent research activities.
- Make study findings available to the public to help build public trust in AI.
Successful piloting of the Center could be made possible by passage of an equivalent bill to S.893 in the current Congress. This is a critical first step in supporting this work. In March 2021, the S.893—Tech to Save Moms Act was introduced in the Senate to fund research conducted by National Academies of Sciences, Engineering, and Medicine to understand the role of AI in maternal care delivery and its impact on bias in maternal health. Passage of an equivalent bill into law would enable the National Academies of Sciences, Engineering, and Medicine to conduct research in parallel with HHS to generate more findings and to broaden potential impact.
Conclusion
The United States has the highest rate of maternal health disparities among all developed countries. Yet more than 60% of pregnancy-related deaths are preventable, highlighting a critical opportunity to uncover the factors impeding more equitable health outcomes for the nation as a whole. Legislative support for research to understand AI’s role in addressing maternal health disparities will affirm the nation’s commitment to ensuring that we are prepared to thrive in a 21st century influenced and shaped by next-generation technologies such as artificial intelligence.
From use to testing to deployment, the scaffolding for responsible integration of AI into high-risk use cases is just not there.
The Federation of American Scientists supports Congress’ ongoing bipartisan efforts to strengthen U.S. leadership with respect to outer space activities.
By preparing credible, bipartisan options now, before the bill becomes law, we can give the Administration a plan that is ready to implement rather than another study that gathers dust.
Even as companies and countries race to adopt AI, the U.S. lacks the capacity to fully characterize the behavior and risks of AI systems and ensure leadership across the AI stack. This gap has direct consequences for Commerce’s core missions.