Creating an Advanced Manufacturing Collaborative for PPE and Other Medical Device Supplies
Summary
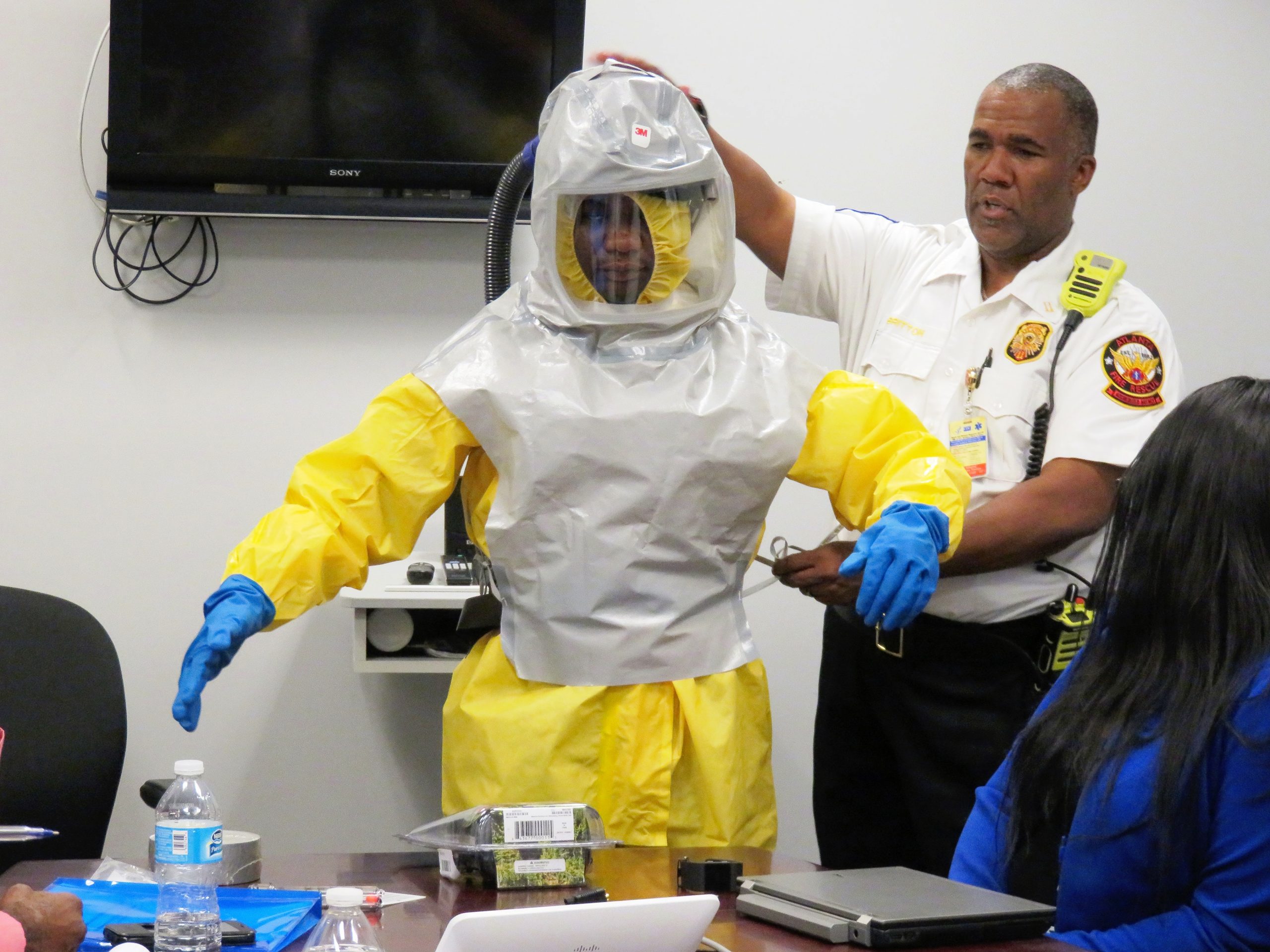
Personal Protective Equipment (PPE) is a critical component of medical care that ensures the safety of both the patient and the provider, as well as the general public. During the COVID-19 pandemic, a global shortage of PPE left many providers insufficiently protected, resulting in infection, increased spread, and even the deaths of providers. To assist, the World Health Organization urged for a 40% increase in production. Treatment of those infected was further hampered by critical shortages of necessary medical supplies such as ventilator parts. The fragility of the supply chain also left civilians without immediate access to PPE, and later widespread use of disposable masks has created a significant environmental hazard. Innovation in PPE has remained stagnant and reliant on single use options which are vulnerable to manufacturing shortcomings and harmful to the environment. This need for improvement also applies directly to other medical equipment, where focus has largely been on single use parts. A collaborative panel and acting body is needed to drive changes forward for the current pandemic, next pandemic, the next critical part shortage, the next wildfire, or even for our agricultural workers who use protective gear every day but still face harmful exposures while ensuring our collective safety.
To drive innovation in PPE and medical parts, there is a need to align regulatory bodies and bridge the gap between regulation and research and development. Collaboration between federal, private, and academic entities is essential. Recently the Federal Drug Administration (FDA), Department of Veterans Affairs (VA), National Institutes of Health (NIH), and America Makes formed a COVID-19 response public-private partnership which addresses some – but not all – of these issues. In particular, reusable equipment is excluded, despite its numerous benefits such as allowing hospitals to ensure availability of equipment on demand and protecting the broader population.
The next administration should target the shortcomings of PPE and single use medical parts more broadly by creating a cross-agency collaboration center for PPE and medical device innovation that focuses on improving efficacy of PPE; stimulating new designs including reusable options; fostering collaborations for the design, research, and manufacture of improved medical parts; and identifying ways to ramp up manufacturing during times of crises while maintaining optimal safety of such equipment.
To secure the U.S. bio-infrastructure, maintain global leadership in biotechnology, and safeguard American citizens from emerging threats to their privacy, the federal government must modernize its approach to human genetic and biological data.
From use to testing to deployment, the scaffolding for responsible integration of AI into high-risk use cases is just not there.
The Federation of American Scientists supports Congress’ ongoing bipartisan efforts to strengthen U.S. leadership with respect to outer space activities.
By preparing credible, bipartisan options now, before the bill becomes law, we can give the Administration a plan that is ready to implement rather than another study that gathers dust.