Establishing a National Endemic Disease Surveillance Initiative (NEDSI)
Summary
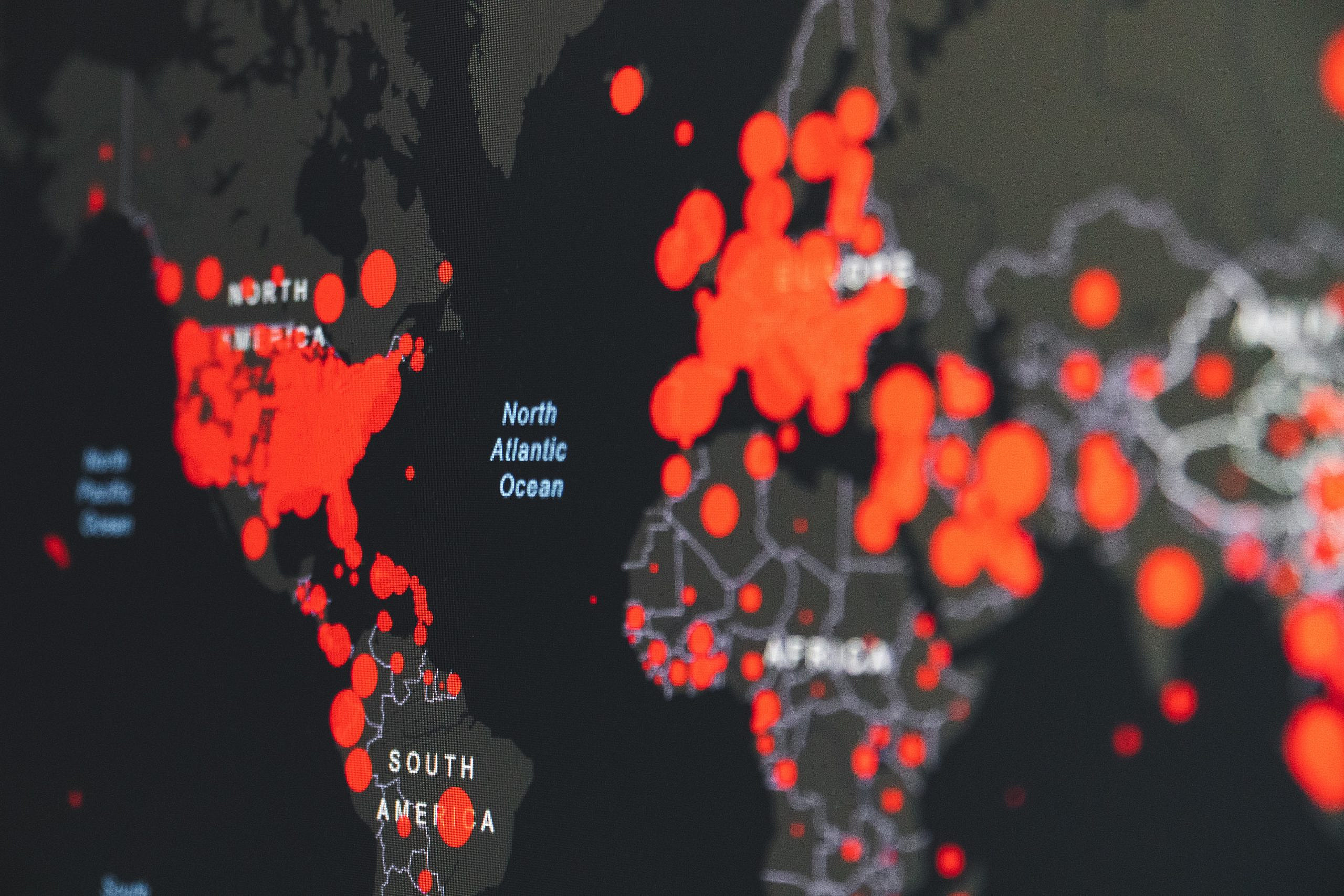
Global pandemics cause major human and financial losses. Our nation has suffered nearly a million deaths associated with COVID-19 to date. The Congressional Budget Office estimates that COVID-19 will cost the United States $7.6 trillion in lost economic output over the next decade. While much has rightly been written on preventing the next pandemic, far less attention has been paid to mitigating the compounding effects of endemic diseases. Endemic diseases are consistently present over time and typically restricted to a defined geographic region. Such diseases can exacerbate pandemic-associated financial losses, complicate patient care, and delay patient recovery. In a clinical context, endemic diseases can worsen existing infections and compromise patient outcomes. For example, co-infections with endemic diseases increase the likelihood of patient mortality from pandemic diseases like COVID-19 and H1N1 influenza.
Accurate and timely data on the prevalence of endemic diseases enables public-health officials to minimize the above-cited burdens through proactive response. Yet the U.S. government does not mandate reporting and/or monitoring of many endemic diseases. The Biden-Harris administration should use American Rescue Plan funds to establish a National Endemic Disease Surveillance Initiative (NEDSI), within the National Notifiable Disease Surveillance System (NNDSS), to remove barriers to monitoring endemic, infectious diseases and to incentivize reporting. The NEDSI will support the goals of the Centers for Disease Control and Prevention (CDC)’s Data Modernization Initiative by providing robust infection data on a typically overlooked suite of diseases in the United States. Specifically, the NEDSI will:
- Provide healthcare practitioners with resources to implement/upgrade digital disease reporting.
- Support effective allocation of funding to hospitals, clinics, and healthcare providers in regions with severe endemic disease.
- Prepare quarterly memos updating healthcare providers about endemic disease prevalence and spread.
- Alert citizens and health-care practitioners in real time of notable infections and disease outbreaks.
- Track and predict endemic-disease burden, enabling strategic-intervention planning within the CDC and with partner entities.
Challenge and Opportunity
The COVID-19 pandemic highlighted the need for a multilevel approach to addressing endemic diseases. Endemic diseases are defined as those that persist at relatively stable case numbers within a defined geographic region. Though endemic diseases are typically geographically restricted, changes in population movement, population behaviors, and environmental conditions are increasing the incidence of endemic diseases. For example, Valley fever, a fungal respiratory disease endemic to the California Central Valley and the American Southwest, is predicted to spread to the American Midwest by 2060 due to climate change.
Better preparing the United States for future pandemics depends partly on better countering endemic disease. Effective patient care during a pandemic requires clinicians to treat not only the primary infection, but also potential secondary infections arising from endemic pathogens taking advantage of a weakened, preoccupied host immune system. Though typically not dangerous on their own, secondary infections from even common fungi such as Aspergillus or Candida can become deadly if the host is pre-infected with a respiratory virus. On the individual level, secondary infections with endemic diseases adversely impact patient recovery and survival rates. On the state level, secondary infections impose major healthcare costs by prolonging patient recovery and increasing medical intervention needs. And on the national level, poor endemic-disease management in one state can cause disease persistence and spread to other states.
Robust surveillance is integral to endemic-disease management. The case of endemic schistosomiasis in the Sichuan province of China illustrates the point. Though the province successfully controlled the disease initially, decreased funding for disease tracking and management—and hence lack of awareness and apathy among stakeholders—caused the disease to re-emerge and case numbers to grow. During active endemic-disease outbreaks, comprehensive data improves decision-making by reflecting the real-time state of infections. In between outbreaks, high-quality surveillance data enables more accurate prediction and thus timely, life-saving intervention. Yet the U.S. government mandates reporting and/or monitoring of relatively few endemic diseases.
Part of the problem is that improvements are needed in our national infrastructure for tracking and reporting diseases of concern. Approximately 95% of all hospitals within the United States use some form of electronic health record (EHR) keeping, but not all hospitals have the same resources to maintain or use EHR systems. For example, rural hospitals generally have poorer capacity to send, receive, find, and integrate patient-care reports. This results in drastic variation in case-reporting quality across the United States: and hence drastic variation in availability of the standardized, accurate data that policy and decision makers need to maximize public health.
With these issues in mind, the Biden-Harris administration should use American Rescue Plan (ARP) funds to establish a National Endemic Disease Surveillance Initiative (NEDSI) within the CDC’s National Notifiable Disease Surveillance System (NNDSS). Fighting an individual pandemic disease is difficult enough. We need better systems to stop endemic diseases from making the battle worse. Implementing NEDSI will equip decision makers with the data they need to respond to real-time needs— thereby protecting our nation’s economy and, more importantly, our people’s lives.
Plan of Action
To build NEDSI, the CDC should use a portion of the $500 million allocated in the ARP to strengthen surveillance and analytic infrastructure and build infectious-disease forecasting systems. NEDSI will support the goals of the CDC’s Data Modernization Initiative by allocating resources to implement and/or upgrade digital-disease reporting capabilities needed to obtain robust infection data on endemic diseases. Specifically, NEDSI would strive to minimize healthcare burdens of endemic diseases through the following four actions:
- Disease monitoring. NEDSI will identify and track notable endemic infectious diseases for each state, including but not exclusive to (i) existing infectious diseases with historical presence and/or relevance, and (ii) infectious diseases that disproportionately impact particular workers. For example, Valley fever disproportionately impacts those employed in outdoor occupations related to ground/soil work (such as agricultural workers, solar farmers, construction workers, etc.). Endemic-disease reporting under NEDSI will follow reporting templates and frameworks that have already been developed by the NNDSS, but will also include information on co-infections (i.e., whether a reported endemic-disease case was a primary, secondary, or higher-order infection).
- Disease notification. As part of monitoring, case-report numbers that rise above historical norms will be automatically flagged for alerts to community members, health-care providers, public-health officials, and other stakeholders.
- Alerts to community members will be geotargeted (for example, by city, county, or region), enabling residents and travelers in endemic zones to take precautions. Alerts will be text-message-based and include resource links vetted by public-health experts.
- Alerts to health-care providers will contain links to resources providing the latest information on accurate diagnosis and appropriate treatment of the disease in question. This will allow providers to quickly identify emerging cases of the disease, as well as to prepare for above-average use/need of particular treatments and equipment.
- Alerts to public-health officials will help shape recommendations for travel restrictions, emergency-funding requests and allocations, and rapid-response resources.
- Disease prediction. NEDSI will work with the CDC and the National Institutes of Health (NIH) to build an endemic-disease prediction model that ranks the severity of current and anticipated endemic-disease burden by geographic region in the United States, enabling proactive intervention against emerging threats.
- Model insights will be shared with the Federal Emergency Management Agency (FEMA) and state health departments to inform allocation of funds (e.g., from the federal-to-state and state-to-county levels) to support public health.
- Key model insights could also be posted on the CDC’s website and transmitted in notices to regional public-health officials and healthcare practitioners, especially when predicted risks and infection trends are high.
- Data underlying the model should be made publicly available and accessible to support external disease-modeling and -prediction efforts.
- In alignment with priorities of the Data Modernization Initiative and the American Pandemic Preparedness Plan, the CDC could also consider offering financial assistance (e.g., through grants or cooperative agreements) to external research efforts conducted in partnership with NEDSI and/or using NEDSI data. NEDSI and NNDSS should work to identify key research targets and promote them appropriately in Notices of Funding Opportunities.
- Health education. The NNDSS, utilizing data and model outputs from NEDSI, should prepare quarterly memos synthesizing key information related to endemic diseases in the United States, including (i) summary statistics of endemic-disease case numbers and co-infections by state and county; (ii) an up-to-date list of available treatments, medications, and therapies for different endemic diseases, and (iii) predicted disease trends for coming months and years. Memos should be published digitally and archived on the CDC website. Publication of each memo should be accompanied by a digital campaign to help spread the resource to healthcare practitioners, public-health authorities, and other stakeholders. NEDSI representatives should also prioritize participation in disease-specific research/clinical conferences to ensure that the latest scientific findings and developments are reflected in the memos.
Conclusion
Despite the clear burdens that endemic diseases impose, such diseases are still largely understudied and poorly understood. Until we have better knowledge of immunology related to endemic-disease co-infections, our best “treatment” is robust surveillance of opportunistic co-infections—surveillance that will enable proactive steps to minimize endemic-disease impacts on already vulnerable populations. Establishing a National Endemic Disease Surveillance Initiative within the National Notifiable Disease Surveillance System will close a critical gap in our nation’s disease-monitoring and -reporting infrastructure, helping reduce healthcare burdens while strengthening pandemic preparedness.
NEDSI, like other systems standardizing and streamlining disease reporting, will allow healthcare practitioners to efficiently—and in some cases, automatically—share data on endemic diseases. Such real-time, consistent data are invaluable for informing public-health responses as well as future emergency planning.
An ounce of endemic-disease prevention is worth far more than a pound of cure—and effective prevention depends on effective monitoring. Research shows that endemic diseases account for an alarming number of co-infections with COVID-19. These co-infections have detrimental impacts on patient outcomes. Further, population growth and migration trends are increasing transmission of and exposure to endemic diseases. Mitigating the severity of future epidemics and pandemics hence requires near-term investment in endemic-disease monitoring.
Yes: even in non-pandemic times, co-infections represent a major risk for the immunocompromised and elderly. AIDS patients succumb to secondary infections as a direct result of becoming immunocompromised by their primary HIV infection. Annual flu seasons are worsened by opportunistic co-infections. Monitoring and tracking endemic diseases and their co-infection rates will help mitigate existing healthcare burdens even outside the scope of a pandemic.
Due to a combination of funding challenges and lack of research progress/understanding, endemic-disease monitoring was only recently identified as a crucial gap in overall infectious disease preparedness. But now, with allocated funds from the American Rescue Plan to strengthen surveillance and infectious-disease forecasting systems, there is a historic opportunity to invest in this important area
As people wait for this catastrophic grid failure to be remedied, much of southeast Texas, which includes Houston, is enduring dangerous, extreme heat with no air conditioning amid an ongoing heatwave.
The federal government plays a critical role in scaling up heat resilience interventions through research and development, regulations, standards, guidance, funding sources, and other policy levers. But what are the transformational policy opportunities for action?
Comprehensive heat safety standards are essential to mitigate the impacts of climate change on farmworkers and ensure the sustainability and resilience of agricultural operations.
Public deliberation, when performed well, can lead to more transparency, accountability to the public, and the emergence of ideas that would otherwise go unnoticed.